Lymphoma and its types
According to histological classification, lymphoma is divided into two broad groups:
Mediastinal lymphoma and fluid in the lungs
- B cell;
- T cell.
According to the classification according to the clinical picture, lymphomas are represented by mediastinal lymphosarcoma, multiple and alimentary lymphosarcoma, and lymphocytic leukemia in cats. MALT lymphoma, or its extranodal form, consisting of marginal zone cells, stands apart. It occurs more often as a pathology of the stomach and is practically not diagnosed in the early stages.
In the practice of a veterinary oncologist, there are indolent and aggressive lymphomas. The first option develops slowly, calmly and, with timely treatment, has a favorable prognosis. The second type quickly spreads throughout the body, covers a wide area of internal organs, requires immediate treatment and has a poor prognosis.
What is lymphoma?
Lymphoma is a lesion of the immune system and internal organs, in which altered cells accumulate, disrupting tissue function.
The tumor develops in the lymphatic system, which helps us fight infections and other diseases. The lymph circulating in it washes all the cells of the body and delivers the necessary substances to them, taking away waste. In the lymph nodes located throughout its network, dangerous substances are neutralized and removed from the body. The lymphatic system complements the circulatory system and helps fluids move throughout the body. Unlike blood, the speed of which is set by the “pump” - the heart, lymph slowly circulates on its own.
Etiology and pathogenesis: mechanism of tumor occurrence
The first on the list of causes that provoke the development of lymphomas in cats is the RNA-containing leukemia virus (FeLV), which is transmitted by contact, in utero, with saliva, and blood from a sick animal to a healthy one. The natural reservoir of this disease is present in a flock of stray cats, so lymphoma is often found in free-ranging animals that have the opportunity to come into contact with stray cats.
Other reasons include:
- the effect of heavy metal salts on the body;
- ionizing radiation;
- unfavorable environmental conditions in the place where the cat lives.
The pathogenesis of development is complex, its essence is that under the influence of a provoking factor, lymphocytes change, their genetic structure is transformed. Subsequently, abnormalities in the DNA structure worsen, control over the correct division of cells is lost, as a result of which they begin to divide uncontrollably, forming a tumor.
With lymphocytic leukemia, the bone marrow is involved in the pathological process; through the blood and lymph flow, malignant cells are spread throughout the body, which provokes the formation of new tumors.
Incidence of non-Hodgkin's lymphomas (NHL)
More than 90% of NHL is diagnosed in adult patients. Most often, NHL occurs between the ages of 60 and 70 years. The risk of developing this tumor increases with age.
The lifetime personal risk of developing NHL is approximately 1 in 50.
Since the beginning of the 70s, there has been an almost twofold increase in the incidence of NHL. This phenomenon is difficult to explain. This is mainly associated with infection caused by the human immunodeficiency virus. Part of this increase can be attributed to improved diagnostics.
Since the late 90s, there has been a stabilization in the incidence of NHL.
NHL is more often detected in men compared to women.
In 2002, 5,532 cases of NHL in adult patients were identified in Russia.
In the United States in 2004, according to preliminary data, 53,370 cases of NHL in adults and children are expected.
Clinical picture of lymphoma in cats
Symptoms depend on the type of lymphoma (lymphosarcoma) and have a broad clinical picture. But the general signs look like this:
- lethargy, apathy;
- weight loss;
- fast fatiguability.
That is, although a cat is normally calm for most of the day, in a sick animal the malaise manifests itself especially acutely. And an attentive owner will notice changes in her behavior quickly.
With mediastinal lymphosarcoma, severe difficulty breathing appears, the cat's posture is unnatural, forced with an elongated neck in order to capture more air. The reason for this is the formation of a tumor of the thymus gland and compression of the lungs by the neoplasm. When the thymus is damaged, fluid also accumulates in the chest cavity, which puts even more pressure on the lung tissue and makes breathing difficult.
The gastrointestinal tract is affected by alimentary lymphosarcoma, clinical signs are nonspecific - vomiting, constipation, diarrhea. The tumor forms on the mesenteric lymph node, stomach or intestines. With extensive lesions, intestinal obstruction forms, this is a signal for urgent surgical intervention.
Multiple (diffuse) lymphomas in a cat’s body can be suspected by enlarged lymph nodes throughout the body. During the examination, damage to the spleen and liver is diagnosed, anemia develops, the number of leukocytes in the blood changes (leukocytosis - increase, leukopenia - decrease).
Risk factors for non-Hodgkin's lymphoma
Risk factors may be genetic (inherited), lifestyle-related, or environmental.
Age is the most important risk factor for NHL. Most cases of NHL are diagnosed in people over 60 years of age.
Congenital defects of the immune system not only predispose to infections, but also increase the risk of developing NHL in children and young adults.
Obesity may increase the risk of NHL.
Radiation increases the risk of leukemia, thyroid cancer, and NHL. Patients who received radiation therapy for cancer later have an increased risk of developing NHL. This risk is further increased when a combination of chemotherapy and radiation is used.
Benzene, herbicides, and insecticides are associated with an increased risk of NHL.
Acquired immunodeficiency caused by the use of various drugs in organ transplant patients increases the risk of developing NHL.
Human immunodeficiency virus infections are associated with an increased risk of some types of NHL.
Epstein-Barr virus is associated with an increased risk of developing Burkitt's lymphoma and other lymphomas, especially in people with AIDS.
The bacterium Helicobacter pylori , which causes stomach ulcers, can also lead to lymphoma of the same location.
Elimination (where possible) of known risk factors can help to prevent this disease to a certain extent.
Secrets of pathology diagnostics at the RosVet VC
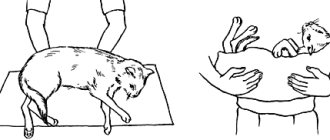
When a cat is admitted with suspected lymphoma, diagnosis is a multi-step process. First, a veterinary oncologist conducts an external examination of the skin and mucous membranes, palpates the area of superficial lymph nodes, evaluates the animal’s appearance, its fatness and the quality of its coat.
Be sure to test the blood for carriage of the feline leukemia virus.
Laboratory blood tests reveal the presence/absence of anemia (drop in hemoglobin level), note the level of leukocytes and enzymes in the blood serum (lactate dehydrogenase, alkaline phosphatase, AlT, AST).
Improvements after chemotherapy for mediastinal lymphoma.
Ultrasound allows you to assess the size and condition of the internal lymph nodes in the abdominal cavity, thymus and lungs.
If altered lymph nodes are detected, cytological diagnostics are prescribed to find out the reason for their enlargement and the presence/absence of tumor cells.
For a biopsy, which is performed in an open manner, it is better to take a whole lymph node, so immunohistochemical and histological analysis will be more accurately carried out.
It is important to understand! All diagnostic procedures must be carried out. This is the only way to make a correct diagnosis, draw conclusions about the severity of the tumor process and develop optimal treatment for each patient with lymphoma admitted to the RosVet EC.
Lymphoma stages
Immediately after detecting the disease, doctors determine its stage - find out how far it has spread and what tissues it has damaged. This information is extremely important for specialists, since it allows not only to understand the patient’s prognosis, but also to select the most appropriate treatment for him.
Stages of Hodgkin lymphoma:
I
: Changed cells are found in only one group of lymph nodes or one lymphoid organ, such as the tonsils.
II
: they are present in 2 or more groups of lymph nodes located on one side of the diaphragm, or have spread from one damaged lymph node to an adjacent organ.
III
: lymphoma cells are present in the lymph nodes on both sides of the diaphragm;
or not only in the lymph nodes above the diaphragm, but also in the spleen. IV
: The disease has spread to at least one organ outside the lymphatic system, such as the liver, bone marrow, or lungs.
Stages of non-Hodgkin's lymphomas:
I
: altered cells are found only in 1 group of lymph nodes or one lymphoid organ, for example, tonsils;
or in 1 area of one organ outside the lymphatic system. II
: they are present in 2 or more groups of lymph nodes on 1 side of the diaphragm;
either in the lymph nodes and 1 area of an adjacent organ, or in another group of lymph nodes on the same side of the diaphragm. III
: lymphoma cells are present in the lymph nodes on both sides of the diaphragm;
or they are present in both the lymph nodes above the diaphragm and the spleen. IV
: The disease has spread to at least one organ outside the lymphatic system, such as the liver, bone marrow, or lungs.
What is the basis for the treatment of malignant tumors?
The basis of treatment for lymphomas is chemotherapy. Various schemes have been developed, their principle of action is based on the introduction of cytotoxic drugs, which should destroy all incorrectly and rapidly dividing cells.
The disadvantage of chemotherapy is that healthy cells, including bone marrow, gonads, and internal organs, are also exposed to toxic substances. Therefore, the dosage of medications is calculated strictly individually.
Cats with lymphoma should be closely monitored by their treating veterinary oncologist. Regularly monitor the level of leukocytes and enzymes in the blood, and monitor the growth or disappearance of the tumor during remission of the disease.
Types of lymphomas
Doctors distinguish 2 main classes of them:
- Hodgkin's lymphoma, or lymphogranulomatosis
: Most often starts in the lymph nodes of the upper body - in the chest, neck or armpits. It usually spreads to various lymph nodes through the lymphatic vessels, but in rare cases, in later stages it enters the bloodstream and spreads to other parts of the body, such as the liver, lungs or bone marrow. This diagnosis is made when special cells are identified in the body - Berezovsky-Reed-Sternberg, which are modified B-lymphocytes.
- TO non-Hodgkin's lymphomas
include all other types of the disease - there are about 30 of them. Each of them has its own special characteristics: the location of the primary tumor, the structure and speed of development.
Disease prognosis and life expectancy
Most lymphomas respond well to chemotherapy; modern drugs cause minimal harm to healthy cells, so treatment can be carried out over a long period of time. This allows you to achieve stable remission of the disease.
Cats with lymphosarcoma live more than 3 years in 15% of cases, about 2 years - only 30% of animals, and up to a year in 65% of oncologist's patients. The earlier cancer pathology was detected, the more fully diagnostic and therapeutic measures were carried out, the higher the likelihood of increasing the cat’s life expectancy.
The owner cannot independently diagnose lymphoma in a cat. But if the pet begins to behave unusually, it develops weakness, general malaise, and the animal visually loses its healthy appearance - you must not hesitate! Timely contacting the RosVet EC is the key to rapid detection of a malignant tumor. Call 24 hours a day and make an appointment with a veterinary oncologist. The clinic operates 24 hours a day; if necessary, a visiting team can come to your home.
Is lymphoma cancer?
Official medicine in Russia and some other countries refers to cancer as malignant tumors - life-threatening neoplasms that develop in epithelial cells contained in the skin or mucous membranes and lining the internal surface of organs.
Lymphoma is not a cancer, but an oncological disease. It is formed from lymphocytes, and its cells are also able to divide uncontrollably, accumulate in tissues, disrupting their work, and create additional foci of disease in various parts of the body.
4.Treatment
Once the diagnosis is established and confirmed, a standard oncological treatment regimen is prescribed, usually with surgical removal of foci of malignant lymphocyte accumulation and mandatory subsequent chemotherapy. Currently, the possibilities of innovative treatment methods (immunotherapy, HIFU therapy, etc.) are being intensively and effectively studied, which gives grounds for reasonable optimism in terms of prospects.
It must be emphasized that the prognosis for intestinal lymphoma (as with any other oncological diseases) critically depends on the timely detection and identification of pathology, especially since in this case early reliable diagnosis is quite possible. Therefore, if you have any combination of the symptoms described above, you should consult a doctor immediately.
References
- Al-Radi, L.S., Baryakh, E.A., Belousova, I.E. Clinical guidelines for the diagnosis and treatment of lymphoproliferative diseases. Association of Oncologists of Russia, 2014. - 296 p.
- Multiple myeloma. Clinical recommendations. Association of Oncologists of Russia, 2021. - 222 p.
- Lifshits, V.M., Sidelnikova, V.I. Medical laboratory tests. - M.: Triad X, 2007. - 312 p.
- Burtis, C. Textbook of clinical chemistry and molecular diagnostics Saunders, 2006. - 555 p.
Signs of development of intestinal lymphoma:
- lack of appetite;
- unusual drowsiness;
- rapid weight loss;
- swelling and enlargement of lymph nodes;
- periodic vomiting;
- diarrhea, presence of blood streaks in the stool;
- abdominal pain and bloating.
If any of these signs are observed, and even more so if they are combined, you need to invite a veterinary oncologist for an initial examination of the pet and the appointment of further diagnostics.
Prospects
The prognosis for the diagnosis of feline lymphosarcoma depends on a large number of factors, the affected organs, the stage of the oncological process and the timeliness of treatment.
The average life expectancy of animals with lymphoma without an appropriate course of chemotherapy is 4-6 weeks.
If the tumor responds well to chemotherapy and there is a positive trend in the course of the disease, the animal's lifespan can be extended to an average of 3 years. In the presence of FeLV and/or FIV virus carriage, lack of treatment, as well as poor response of lymphoma to chemotherapy drugs, the prognosis may worsen to unfavorable.
MALT lymphomas (tumors of mucosal associated lymphoid tissue) are B-cell non-Hodgkin's lymphomas (NHLs) of marginal zone origin, along with marginal zone lymphomas of the spleen and nodal marginal zone lymphomas. Moreover, MALT lymphomas are the most common type of marginal zone lymphomas, accounting for 50–70% of all cases [1, 2].
It should be noted that lesions of the gastrointestinal tract in NHL are observed, according to the literature, in 4-25% of cases of all extranodal localizations of the pathological process. At the same time, the number of NHL among all malignant neoplasms of the gastrointestinal tract (GIT) ranges from 1 to 10%. MALT lymphomas account for 6–11% of NHL in the gastrointestinal localization [2–4].
The most common form of MALT lymphoma of the gastrointestinal tract is gastric MALT lymphoma, which accounts for 30-40% of all cases of this disease. Intestinal lesions are found in 4-8% of patients with MALT lymphomas, and the disease occurs in the small intestine 2 times more often than in the large intestine. Among extraintestinal localizations of MALT lymphomas, lesions of the head and neck, skin, lungs, thyroid and mammary glands are of leading importance [5–7].
The main role in the pathogenesis of MALT lymphomas, according to modern concepts, is assigned to a chronic inflammatory process, leading to the accumulation of autoreactive lymphoid tissue, repeated division of B cells with an increase in the number of cytogenetic disorders, which leads to the development of malignancy [2, 6]. The main causes of the chronic inflammatory process as an inducer of the development of MALT lymphomas are considered to be autoimmune processes and the presence of persistent infection. For lymphomas localized in the gastrointestinal tract, a connection between Helicobacter pylori
and the risk of developing gastric MALT lymphomas (
H. pylori
in gastric MALT lymphoma is detected in 90% of patients).
In addition, a correlation has been identified between the presence of Helicobacter jejuni
and the development of duodenal lymphomas [5, 6, 8]. There are reports indicating an increased likelihood of the disease in patients with chronic viral hepatitis C [8]; provides data on the possibility of the appearance of intestinal lymphomas against the background of celiac disease [9].
From the point of view of the clinical picture of the disease, MALT lymphomas of the gastrointestinal tract are characterized by a long asymptomatic course and can also be accompanied by a number of nonspecific symptoms. When the stomach is affected, the disease can occur under the guise of gastritis; when localized in the intestines, the main complaints of patients may be a feeling of discomfort in the abdomen, moderate periodic pain, and dyspepsia. In some cases, signs of malabsorption appear [2, 6, 10, 11].
Among the complications of intestinal MALT lymphomas, the leading role is played by intestinal obstruction, which, according to some data, develops in 70-80% of patients. Other acute life-threatening conditions such as tumor perforation and bleeding are relatively rare (1-3% of cases) [2, 4, 7].
The principles of treatment of MALT lymphomas of the gastrointestinal tract depend on the location of the formation and the stage of the malignant process. When the stomach is affected, the main treatment method is anti-Helicobacter therapy, which in 50-80% of cases allows one to achieve remission. In case of ineffectiveness of eradication therapy, as well as in case of a high degree of malignancy of the tumor, combined treatment (chemotherapy, radiation therapy, surgery) is recommended [3, 5, 6]. When lymphoma is localized in the intestine, surgical techniques, radiation, mono- and polychemotherapy, and combined treatment are used. The role of surgical treatment of lymphomas of the small and large intestine is especially high due to a significant proportion of complications requiring urgent surgical intervention [1, 2, 8].
We have experience in treating a patient with MALT lymphoma of the small intestine, which was first identified due to tumor perforation and the development of the clinical picture of peritonitis. Here is our observation.
Patient P., 70 years old, was hospitalized on April 16, 2012 in the surgical department of the Central Clinical Hospital of the Federal Customs Service of Russia (CCG FCS) with complaints of severe abdominal pain, worsening with changes in body position, cough, nausea, and general weakness.
From the anamnesis it is known that from August 26, 2010 to September 9, 2010, the patient was hospitalized in the therapeutic department of the Central Clinical Hospital of the Federal Customs Service for fever and anemia of unknown origin. The fever first appeared in August 2010 and was characterized by evening rises in body temperature to 39.0–39.5 °C and night sweats. The hemoglobin level in the blood during hospitalization was 98 g/l. Since 1980, the patient was diagnosed with chronic viral hepatitis C, and since 1989 - celiac disease. After a course of anti-anemic therapy, the patient was voluntarily discharged for outpatient treatment. However, due to ongoing fever, on September 20, 2010, the patient was hospitalized at an outside medical facility, where during the examination, hematological, oncological and rheumatological causes of the disease were rejected. Enteritis not specified in the context of celiac disease or an abscess of unknown localization were identified as a possible factor causing the fever. The patient refused further examination at this healthcare institution and on November 11, 2010 she was again admitted to the therapeutic department of the Central Clinical Hospital of the Federal Customs Service with continuing nightly fever. At the same time, the patient noted that over the previous 3 months she had lost 10 kg. In the results of laboratory tests, attention was paid to leukocytosis (up to 12 thousand) with a band shift (up to 22%), hypoproteinemia (50 g/l), and a positive reaction to occult blood in a stool test. During the hospital stay, esophagogastroduodenoscopy (superficial atrophic gastritis, signs of atrophic duodenopathy), colonoscopy (single diverticulum of the colon), computed tomography of the abdominal cavity and pelvis (signs of enteritis, quantitative enlargement of the lymph nodes (LN) of the mesentery of the small intestine, hepatomegaly, fatty hepatosis), enterography (no filling defects were detected). The patient was also repeatedly examined by specialist consultants from external therapeutic departments. Among the therapeutic measures, the patient underwent massive antibiotic therapy with a change in antibacterial drugs (ceftriaxone, amikacin, tienam). After prescribing each of the drugs, positive dynamics were observed in the form of normalization of body temperature and a decrease in leukocytosis, however, after discontinuation of the antibiotic, the symptoms returned. Due to this picture of the disease, therapy with prednisolone ex juvantibus
, during which regression of fever was obtained. The patient was discharged on December 30, 2010 for outpatient observation with recommendations to continue taking prednisolone. Diagnosis: celiac disease with maldigestion syndrome of the third degree, secondary iron deficiency anemia of moderate severity, chronic viral hepatitis C, class A, multinodular euthyroid goiter of the second degree, kidney cysts, ciscirculatory encephalopathy of the second degree, atherosclerosis of the brachycephalic arteries, autonomic dystonia syndrome.
From January 12, 2011 to January 19, 2011, a control examination was carried out in the therapeutic department of the Central Clinical Hospital of the Federal Customs Service. Among the patient's complaints, moderate general weakness remained; her body temperature remained normal while taking steroid hormones. A weight gain of 2 kg was noted. Upon discharge, it was recommended to continue taking prednisolone.
During this hospitalization in the surgical department of the hospital, upon examination of the patient, pronounced pain on palpation was determined in all parts of the abdomen, which was moderately swollen. Positive symptoms of peritoneal irritation were detected in all sections. Blood tests revealed leukocytosis (16.7 thousand), hypoproteinemia (44 g/l). Based on the results of a chest x-ray and a plain x-ray of the abdominal cavity, right-sided lower lobe pneumonia was diagnosed. No data were obtained to confirm horizontal fluid levels, intestinal arches, or free gas in the abdominal cavity.
Considering the clinical picture of diffuse peritonitis, the patient was operated on urgently after short-term preparation in the intensive care unit. Surgical intervention began with diagnostic laparoscopy. When examining the abdominal cavity in all parts, there is up to 500 ml of purulent turbid effusion, fibrin overlay. The loops of the small and large intestines are hyperemic, edematous, sluggishly peristalt, and moderately distended. Taking into account the prevalence and severity of the process, it was decided to perform an access conversion. A midmedian laparotomy was performed. No pathology was detected in the liver, gallbladder, pancreas, stomach, or colon. When examining the small intestine at a distance of 1.5 m from the ileocecal angle, a circular thickening of the intestinal wall of up to 4-5 mm over a distance of 6 cm was discovered without obstruction of patency. In the center of the formation, a perforated hole of up to 2 mm was identified, from which intestinal contents came. In the mesentery of the small intestine, in the projection of the tumor, a package of lymph nodes was identified, enlarged to 2-4 cm, with a soft elastic consistency. Intraoperative diagnosis: perforation of a tumor of the small intestine. Diffuse fibrinous-purulent peritonitis. The following was performed: resection of a section of the small intestine with a tumor with a 20 cm indentation to the sides of the tumor; wedge-shaped resection of the mesentery of the small intestine with lymph nodes. The intestinal stumps are sutured using a hardware suture, a side-to-side anastomosis is performed, the window in the mesentery is sutured with interrupted sutures. A nasointestinal tube was inserted 30 cm into the small intestine. The abdominal cavity was sanitized and drained, and the laparotomy wound was sutured tightly in layers.
The course of the postoperative period was complicated by the presence of community-acquired lower lobe pneumonia in the patient. Detoxification, massive antibacterial therapy, and physiotherapy were carried out. With treatment, the pneumonia resolved. The sutures were removed on the 11th day after surgery, the wound healed by primary intention. A control ultrasound of the abdominal organs revealed no free fluid, streaks, or infiltrates. Body temperature at discharge was within normal limits. Histological examination of the surgical material: large cell lymphoma (MALT lymphoma) of the small intestine with ulceration and perforation of the intestinal wall. No signs of tumor growth were found at the resection margins or mesenteric lymph nodes. In the lymph nodes, nonspecific reactive hyperplasia of the B-cell type is determined. The patient was discharged on May 4, 2012 in satisfactory condition under the supervision of an oncologist at her place of residence.
Thus, the presented case from practice demonstrates not the most typical course of such a rare disease as MALT lymphoma of the small intestine. The patient had very pronounced symptoms for a long time, the nature of which, however, did not allow us to assume and determine lymphoma of the small intestine. And despite the fact that the localization of the pathological process was determined correctly during previous examinations, the nature of the disease was not clarified before the occurrence of a surgical complication. This is primarily due to the low accessibility of the small intestine for standard endoscopic and imaging methods, while techniques such as intestinoscopy and capsule endoscopy remain rare. It is also interesting that the patient has a long history of celiac disease and chronic viral hepatitis C, which are reported to increase the risk of developing intestinal lymphomas.
As a result, it should be noted that various diseases of the small intestine, including MALT lymphoma, necessitate wider implementation of modern endoscopic technologies, which can prevent the development of life-threatening conditions during a long course of the pathological process and facilitate surgical treatment as planned, if any indications for performing the operation.
Symptoms
Depending on the location of the lymphoma, symptoms will vary. Signs of intestinal cancer in a cat do not appear immediately, remaining invisible to humans for a long time. The pet may be lethargic and refuse food. Sometimes there is upset stool and vomiting.
The owner of the animal may confuse these symptoms with poisoning or other disorders without contacting a veterinary clinic. With the development of the pathological process, the symptoms of nutritional lymphoma become more pronounced. Abdominal (intestinal) lymphoma has similar symptoms to other lesions of the digestive system of an infectious or non-infectious type.
The main features are:
- eruption of gastric contents;
- bowel dysfunction (constipation interspersed with profuse diarrhea);
- refusal to eat;
- a sharp decrease in body weight;
- anemia of visible mucous membranes;
- violation of the secretion of glands;
- dehydration due to vomiting or diarrhea;
- change in the condition of the coat (it becomes dull, brittle, lacks shine);
- apathy and lethargy of the pet;
- severe exhaustion.
Caring for a sick cat
Unfortunately, there is no cure for this disease. In some cases, the only solution is to provide additional care to improve the quality of life of the affected animals.
It is important to closely monitor your cat's food and water intake while she is in the recovery phase.
The prognosis of this disease is highly variable and depends on the initial response to treatment, anatomical tumor type, FeLV status, and tumor burden.
If chemotherapy is started, you may need to check your cat regularly. At each visit, your veterinarian will perform blood tests to determine the response to treatment, as well as check the status of any complications arising from the treatment so that necessary adjustments can be made.
If chemotherapy drugs have been prescribed as part of your home treatment, be sure to follow the instructions carefully as chemotherapy drugs are very toxic to human health. Basic precautions include using latex gloves before taking the medicine.
If pain medications for cats have been prescribed, use them with caution and follow all instructions carefully, making sure all family members are familiar with the medication schedule; One of the most preventable pet disasters is drug overdose.
Survival times vary greatly, from several months to less than two years.
Diagnosis of the disease
To make a diagnosis, the doctor conducts a histological examination of the affected lymph node. Sometimes the organ is located in such a place in the body that it is impossible to reach it. In this case, additional research is carried out:
- blood analysis;
- Ultrasound;
- radiography;
- PCR.
The veterinarian must examine the skin and visible mucous membranes and palpate the lymph nodes. If alimentary lymphoma is suspected, an animal stool test may be necessary.