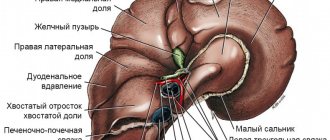
How does the liver work?
The liver is the largest gland of the body, the main task of which is to neutralize and remove poisons from the body (including metabolic products), excess hormones, mediators, and vitamins. To do this she:
- filters out fat-soluble toxins, turning them into water-soluble substances;
- produces enzymes that break down drugs and other chemical compounds.
The more poisons in the body, the heavier the liver. Toxins kill her cells (hepatocytes), and regeneration takes time. While the new cell grows, the load on nearby tissues increases.
If there are too many poisons, hepatocytes can die en masse, then connective tissue appears in their place. Although it closes the hole, it is unable to perform the work of the liver. Intoxication of the body begins, which can cause death.
Other liver functions
Neutralization of poisons is the main, but not the only task of the liver. She:
- Participates in lipid and carbohydrate metabolism.
- Produces proteins, incl. albumins, which carry hormones and other substances to cells.
- Stores minerals, glycogen, triglycerides.
- Activates vitamins.
- Synthesizes substances that are involved in blood clotting.
- Produces bile acids and enzymes.
The liver processes bilirubin, a pigment formed after the breakdown of red blood cells. This is a very toxic substance, which the organ neutralizes and sends as part of bile to digest food. The pigment then passes into the stool and leaves the body.
Excess bilirubin in the blood is the cause of yellowing of the mucous membranes in animals. The pigment is sent not into the bile, but into the plasma, so the stool, to which it gives a dark color, becomes discolored. The urine becomes the color of beer because the bilirubin has to be excreted by the kidneys.
Needs
1 Energy
The body's energy needs can be calculated using the formula: E = 125 W 0.75 kcal/day. E = 523 W 0.75 kJ/day. Where W is body weight in kilograms (2)
The energy requirement of cats at rest is 50–90 kcal per kilogram of body weight per day. (3)
| Cat (1 kg of weight per day) | kcal | kJ |
| Adult, normal | 70-90 | 293-377 |
| Adult, inactive: | 50-70 | 209-293 |
| Pregnancy: | 100-140 | 419-586 |
| Lactation: | 240+ | 1004+ |
| Growth period: | ||
| 10 weeks after birth | 220 | 921 |
| 20 weeks after birth | 160 | 670 |
| 30 weeks after birth | 120 | 502 |
| 40 weeks after birth | 100 | 419 |
Cats' protein needs can be determined in three ways.
- On average, cats need 15 g of protein per MJ of metabolic energy per day (3).
- They are calculated based on actual weight and amount to 1-2 gkg per day multiplied by the metabolic activity indicator.
- The ratio of protein calories to nitrogen is used. Each gram of nitrogen input must provide 150 kcal of energy, so dividing the total calories by 150 gives the grams of nitrogen needed. Multiplying the resulting figure by 6.25 gives the required amount of protein in grams. (4)
3 Liquid
- The amount of fluid entering the body should be from 0.2 to 0.3 ml per kJ, from 1 to 1.2 ml per 1 kcal, plus the volume of losses (vomiting, diarrhea, etc.). (2)
- 30 – 40 ml of liquid per 1 kilogram of body weight. (4)
Energy value of 1 gram of main nutritional components
| Name of components | Energy value | |
| kcal | kJ | |
| Squirrels | 4,2 | 17,58 |
| Carbohydrates | 4,1 | 17,1 |
| Fats | 9,3 | 38,94 |
| Ethanol | 7,1 | 29,6 |
Symptoms of a diseased liver in animals
Failures in the liver negatively affect the functioning of all organs and systems. This explains the first symptoms of the disease - fatigue, bad mood, decreased activity, irritability, aggression. The appetite gradually worsens, the dog suddenly loses weight, thirst appears, and discharge from the eyes appears. The temperature may rise.
Over time, symptoms characteristic of a diseased liver develop:
- yellowing of the mucous membranes of the eyes, mouth, gums;
- digestive problems – vomiting, diarrhea, bloating;
- dark urine;
- seizures and other neurological problems;
- gastrointestinal bleeding due to poor coagulation, the appearance of ulcers;
- accumulation of fluid in the abdomen, due to which one may mistakenly assume that the pet has gained weight (extreme stage, a symptom of imminent death).
Clinical signs of toxic hepatitis
Signs of an acute form of the disease
Symptoms of toxic hepatitis are very variable and in most cases depend on the degree of poisoning and on which particular toxic substance provoked the development of the pathological process.
However, there are also characteristic signs that are common to all types of toxic hepatitis:
- fast fatiguability;
- loss of appetite;
- bitterness in the mouth;
- belching;
- bloating;
- pain in the right hypochondrium;
- yellowing of the sclera, skin and mucous membranes;
- increase in body temperature to 37–38 °C.
Many patients with toxic hepatitis develop a rash on the skin, accompanied by itching of varying intensity, urine becomes the color of dark beer, and stool becomes light-colored with a clay consistency. Often, liver damage is accompanied by an increase in the size of the organ, the appearance of small hemorrhages on the skin, bleeding gums and nosebleeds (a consequence of the destructive effect of toxic substances on the walls of blood vessels). In some cases, lethargy or excessive agitation, hand tremors, and spatial disorientation are observed.
Signs of a chronic form of the disease
As the disease becomes chronic, the symptoms of toxic liver damage become less pronounced. Typically, patients complain of the following symptoms:
- periodic pain in the right hypochondrium, worsening after eating;
- bitterness in the mouth;
- decreased performance;
- fatigue;
- flatulence;
- nausea;
- occasional bouts of vomiting;
- stool disorders;
- hepatosplenomegaly (marked enlargement of the liver and spleen).
During remission, symptoms may subside, but during an exacerbation they reappear.
Causes of liver disease in animals
The liver destroys toxins through oxidative processes, so free radicals accumulate in it. In large quantities they are dangerous because they damage the gland and slow down cell regeneration.
The heavier the poisons that the organ must neutralize, the more free radicals the liver produces, the higher the risk of damage to hepatocytes. The solution is to reduce the cat or dog’s exposure to toxins.
Liver problems in pets are caused by medications and chemicals:
- Anthelmintic drugs. They must be given to prevent the development of parasites, but in no case exceed the dosage.
- Flea and tick medications, tablets are especially dangerous.
- Vaccination. The injection protects the pet from fatal diseases, but creates additional stress on the liver.
- Household chemicals – products for cleaning carpets, floors, furniture.
- Pesticides and herbicides are a problem often faced by pets living in the countryside or in the country.
- Nutritional supplements.
- Heavy metals.
Who's at risk
Liver dysfunction is common in older dogs and cats. Also among the reasons are obesity, prolonged fasting, stress, tattoos, microchips. Liver problems can be caused by:
- pancreatitis;
- oncology of other organs;
- sick kidneys;
- worms;
- viral, bacterial infections;
- autoimmune pathologies;
- hormonal imbalances.
The liver can fail due to a sudden change in nutrition (for example, when switching from natural food to ready-made food), an overdose of vitamins and minerals. Cheap food can cause poisoning.
Some dog breeds have a genetic predisposition to liver disease:
- Dobermans;
- Rottweilers;
- Yorkshire Terriers;
- cocker spaniels;
- Bedlington Terriers;
- West Highland White Terrier.
These breeds have a hereditary condition associated with copper accumulation in the liver. With the help of this substance, iron produces some enzymes, but excess copper causes damage to the proteins that bind it. The result is inflammation of the gland, cirrhosis.
Diagnostics
Diagnosis of toxic hepatitis includes instrumental and laboratory methods that are also used in identifying other acute and chronic liver lesions. During the first medical consultation, a physical examination and history taking are performed. In most cases, this allows you to get a rough idea of the reasons that triggered the development of toxic hepatitis.
Laboratory methods for diagnosing liver damage:
- biochemical blood test - determination of the level of direct, indirect and total bilirubin, alkaline phosphatase, AlT and AST and γ-GTP;
- coagulogram - prescribed to assess the state of the hemostatic system;
- general blood and urine tests;
- tests to exclude the presence of other forms of hepatitis.
Instrumental diagnostic techniques:
- Ultrasound of the abdominal organs;
- liver scintigraphy;
- MRI;
- laparoscopic examination with targeted puncture biopsy of the liver.
Major liver diseases in animals
There are many pathologies that are caused by the liver. Diseases can be divided into 3 groups:
- Inflammatory infectious diseases - liver abscess in cats, leptospirosis, viral hepatitis, adenovirus type 1 in dogs.
- Inflammatory non-infectious – lymphocytic cholangitis in cats, chronic hepatitis in dogs.
- Non-inflammatory – hepatosis in cats, copper accumulation in dogs.
Hepatitis
Most often, dogs encounter infectious (viral) hepatitis - inflammation of the liver. The pathology is difficult, fast, and often ends in the death of the pet. Other types of hepatitis that occurs in animals are caused by worms and bacteria. Inflammation of the liver can be a consequence of diseases of the pancreas and digestive system.
Hepatosis
Hepatosis occurs more often in cats. The pathology develops due to the accumulation of fat in the liver cells, which leads to its degeneration. The disease is a consequence of obesity, hormonal imbalances, and poor nutrition, which cause inflammation of the liver. The pathology is dangerous; if left untreated, it often develops into cirrhosis.
Amyloidosis
The disease is characterized by a disorder of protein metabolism, when amyloid, a fibrous substance, is deposited in tissues and causes cell death. Pathology can affect different organs, incl. liver.
Cirrhosis
The disease develops slowly and usually ends in death. As liver cells die, they are replaced by connective tissue, and it cannot cope with its tasks. The animal dies from intoxication, thrombosis, and internal bleeding.
A characteristic sign of cirrhosis is ascites, the accumulation of fluid in the abdominal cavity. It puts pressure on the diaphragm, causing blood stagnation, ulcers, increased pressure in the liver area, and other problems.
Causes of cirrhosis in animals:
- low-quality food containing poisons;
- deficiency of selenium, pyridoxine, and some other elements;
- hepatitis, hepatosis, inflammation of the gallbladder;
- parasites (pyroplasmosis, toxocariasis);
- plague, enteritis.
Liver cancer
Cancer is a condition where cells begin to divide abnormally and do not die. They displace healthy tissues, but cannot replace them, which leads to the death of the body. Liver cancer often develops as a secondary disease when malignant cells from a tumor located in another part of the body enter the gland.
Less commonly, cancer occurs in the liver itself. It is usually a consequence of cirrhosis. Another reason may be long-term exposure to carcinogenic factors (eg, heavy metals).
Lipidosis
This disease is popularly called fatty liver , since in this case the organ is literally covered with a solid layer of fatty tissue. Contrary to popular belief, lipidosis can be congenital or hereditary. The bottom line is that even with a predisposition, a cat may not suffer from the disease if it eats properly and exercises enough.
Acquired lipidosis is a consequence of a disorder of fat metabolism, that is, not an independent disease, but a component of it. Typically, the diagnosis is made in animals between 2 and 4 years of age. A special risk group includes cats living in stressful environments or those who are overweight. In recent years, veterinarians have begun to argue that lipidosis is more likely to develop in overweight spayed or neutered cats.
The difficulty is that the symptoms of the disease appear gradually. When it becomes obvious to the owner that the cat is sick, it turns out that the liver is severely damaged. This is one of the reasons why your pet should be shown to the doctor on a preventive basis, even if, in your opinion, nothing is bothering him.
Symptoms of lipidosis include:
- Apathy.
- Poor appetite.
- Gradual weight loss.
- Unpleasant, acetone smell from the mouth.
- Increased salivation and vomiting with yellow foam.
- Inflammation of the liver.
- Jaundice, which can cause the cat to fall into a coma.
Note! Quite often, lipidosis develops as a concomitant disease against the background of diabetes mellitus.
Therapy
To treat and restore liver function, the doctor prescribes medications from the following groups:
- Hepatoprotectors (Hepatovet, Hepatolux, Hepasafe) - improve metabolic processes in the liver, increase its resistance to toxins, and stimulate cell regeneration.
- Choleretic drugs (preparations with milk thistle) - accelerate the formation of bile in the liver, promote its removal from the gallbladder to the intestines.
- Sorbents (Simbosorb, EnteroZoo) - absorb toxins, reducing the load on the liver.
For cirrhosis, the doctor may prescribe injections of glucose, insulin, and vitamins. Diuretics will help remove ascites. To relieve inflammation, hormonal drugs are prescribed. Cancer requires chemotherapy and surgery.
Unfortunately, cirrhosis and liver cancer often result in death, but therapy can prolong the life of a pet and relieve pain.
Diet
Treatment of any liver disease involves diet. Proper nutrition will reduce the load on the gland, which promotes recovery, and if healing is not possible, it will improve your well-being. Give food that is light but nutritious, rich in all nutrients. Products should not irritate the digestive tract.
Discuss the diet with your veterinarian. He will recommend the right food if the animal is on a natural diet, and will recommend healthy products. If your dog has copper hepatopathy, your doctor will prescribe a diet low in copper and high in zinc.
Diet and treatment of lipidosis
Diagnosis is carried out on the basis of anamnesis, blood sampling and ultrasound. Once the diagnosis is confirmed, emergency therapy is started to support the liver. In severe condition, animals usually refuse to eat, so they are fed from a syringe or using a nasal tube.
During therapy, the pet is constantly offered food. Appearing appetite indicates an improvement in the condition. When the cat begins to eat, treatment is continued at home. Usually they do not experiment with the diet and transfer the patient to special medicinal foods. During primary rehabilitation, the cat is fed only wet and liquid food. When liver functions are partially restored, the animal is transferred to dry medicated food. The duration of therapy directly depends on the dynamics of the disease. Often, owners have to keep cats on medicated food for life.
Note! When treating lipidosis, veterinarians often resort to the use of homeopathy and herbal remedies.
Prevention
Monitor your pet's diet. Do not feed your dog or cat food from the table. Buy only high-quality, proven food. If your pet is on a natural diet, give raw lean meat, boiled fish, fresh vegetables and fruits. Wipe or steam the greens for better absorption. Avoid sausages, sausages, do not give rotten, bad food.
Other recommendations:
- Remove toxins that may harm the liver. This means that you need to avoid unnecessary pesticides and medications. Avoid frequent cleaning using household chemicals.
- Synthetic vitamins and minerals can be given strictly according to the instructions, without exceeding the course duration and dose.
- Supplement with the antioxidants glutathione, the amino acids N-acetylcysteine (NAC) and S-adenosylmethionine (SAMe). They bind to toxins in the liver before the poisons can damage the gland. Be sure to consider the dosage.
- Get vaccinated against deadly diseases on time.
Natural products
All products must be exceptionally fresh and of high quality. Any blow to the liver and digestive system as a whole can now be disastrous. Food must be warm, room temperature or slightly warmer. Vegetables, fish and meat are pre-cooked.
If after the first days of the diet the cat is recovering, its appetite has improved, the diet can be diversified. If not, continue to give the broth, you can add a little rice or oatmeal broth.
10 foods included in the hepatitis diet:
- light fish or meat broth (it is better to drain the first broth, so it will be less fatty);
- rice decoction;
- oatmeal broth (oatmeal in bags with additives and sugar is definitely prohibited);
- herbal infusions aimed at maintaining the immune system, liver and digestive system;
- boiled chicken breast (start giving at the end of the first week of the diet, chopped, in small portions);
- boiled low-fat fish (except river fish);
- boiled beef (by the end of the first week, minced in a blender or meat grinder);
- low-fat cottage cheese;
- kefir 1%;
- boiled carrots (for better feces formation).
10 foods prohibited for hepatitis:
- fatty fish;
- pork, lard;
- udder (too fat);
- milk (any);
- sour cream;
- vegetables that cause flatulence;
- sugar;
- salt and spices;
- smoked meats;
- roast;
First of all, everything fatty, as well as products containing salt and spices, are prohibited.
The animal must be stimulated with vitamin supplements. Vitamins B, C and K are especially important for liver diseases. When choosing vitamins, it is better to consult a veterinarian.