The kidneys are an important organ for both the human and feline body. With their help, substances harmful to the body are removed. The kidneys play a significant role in the body's metabolic processes. Pathology in the kidneys is a serious metabolic disorder
and contributes to the development of various diseases.
Kidney failure is a disease that affects the functioning of all body systems. But clinical manifestations are visible only when 65-80% of the kidney tissue is already affected. The earlier the disease is detected, the longer the cat will live after proper therapy.
In renal failure, the kidneys perform their main function—excretory—poorly or stop performing altogether. Problems in the excretory system upset the balances:
- Acid-base;
- Water-salt;
- Osmotic.
These disturbances trigger problematic conditions in other internal organs.
Kidney failure occurs more often in cats of the Persian and British breeds, since they are more susceptible to a congenital anomaly - polycystic kidney disease. And this disease provokes chronic renal failure.
Abessinian cats suffer from amyloidosis, which also causes chronic renal failure.
There is no clear opinion about who is more predisposed to the disease – males or female cats.
Treatment of renal failure can be effective only in the initial stage. The prognosis for recovery is significantly reduced if the disease is advanced. If any minor signs of illness appear, you should immediately contact a veterinarian.
The symptoms of kidney failure are similar to those of other diseases, so the cat must be fully examined to establish an accurate diagnosis. You should not give your animal any medications on your own. Only a specialist can treat a pet.
Prevalence of CKD
Chronic kidney disease (CKD) is one of the most common diseases in cats, affecting up to 35% of older cats1-5 and up to 10% of all cats seen in veterinary clinics.6-8 FEDIAF (European Feed Industry Federation) estimates pets), in Europe alone, approximately 9 million cats were affected as of 2010.9 As the cat population is gradually aging, CKD in cats is expected to become the predominant disease over time.
Neutered cats
Before castration, the doctor is obliged to warn the owners of the animal that all sorts of complications may arise after the procedure:
- Obesity;
- Formation of sand and stones;
- Disorders of the urinary system.
Kidney disease in castrated cats can be caused by the following factors:
- Unhealthy eating. Namely, feeding fatty foods, fish, cheap food of dubious origin, food with a high content of proteins, minerals and salts;
- Mixed nutrition. The pet should be fed either natural products or a food mixture. When mixed, improper metabolism occurs, which leads to the formation of stones;
- Lack of water. There should always be water in the cup;
- Lack of mobility;
- Genetic predisposition;
- Pathology;
- Infectious disease;
- Disorders of the gastrointestinal tract.
You need to love your pet, take care of it, feed it properly, consult a veterinarian on time, and then for many years a faithful friend and pet will be nearby, who will brighten up loneliness and give unique moments of tenderness, affection and love, so necessary for man and cat.
Pathophysiology
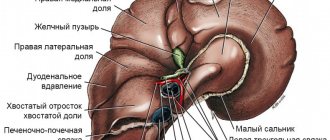
The main function of the kidneys is to constantly filter the blood and excrete urea and other metabolic products, while preventing the loss of water and electrolytes. The structural and functional unit of the kidneys that performs this important function is the nephron (Fig. 1). An indicator of the effectiveness of the kidney filter is the glomerular filtration rate (GFR).
Rice. 1. Functional anatomy of the kidneys; nephron structure
The kidneys perform a number of other important functions in the body, including:
- Maintaining optimal blood pressure
- Maintaining calcium and phosphate levels in the body
- Maintaining a normal number of red blood cells (RBC) in the blood.
In many cases, in cats with this pathology, there is a progressive decrease in the glomerular filtration rate up to azotemia (i.e., an increase in the level of nitrogen-containing substances such as urea and creatinine in the blood), which develops when more than 75% of functioning nephrons die. 13
In cats, CKD is considered a spontaneously progressive disease because, once renal function declines to a certain level, progressive nephron death persists even after the underlying pathology has resolved. Most treatments for CKD in cats are aimed at suppressing the maladaptive mechanisms responsible for the spontaneous progression of the disease.11-13
How to prepare for a kidney ultrasound?
As before an abdominal examination, it is advisable to fast for 10-12 hours before an ultrasound examination of the kidneys, since gas and intestinal contents will make visualization difficult. If your cat has contraindications to a starvation diet, and if it is necessary to perform an ultrasound on your kitten, consult your doctor. Since kidney examinations are rarely done without examining the bladder, it is important that the bladder is full before the ultrasound. Therefore, when preparing, remove the cat's litter box or close access to the toilet 4-5 hours in advance. If urination has been recent, the bladder will be empty, deflated, and it will be impossible to assess the condition of its walls, the presence or absence of urine.
Video with a visual diagnostic veterinarian about ultrasound of kidneys in cats:
When performing a kidney ultrasound, owners place the cat on its back on a special table and hold the front and back legs. The doctor shave the examination site, apply alcohol and acoustic gel to the skin. In large or obese animals, the doctor may apply pressure to the area being examined with a probe for better visualization due to the anatomical location of the kidneys. This may not be very comfortable for the animal, so restraint is important.
Kidney ultrasound is not the only method for diagnosing the disease. The attending physician makes a comprehensive diagnosis, based on the medical history, general condition of the animal, clinical symptoms, examination, ultrasound and laboratory diagnostic results.
(c) Veterinary center for the treatment and rehabilitation of animals “Zoostatus”. Varshavskoe highway, 125 building 1. tel.
8 (499) 372-27-37
Glomerular hypertension and disease progression
In cats with chronic kidney disease, as the number of functioning nephrons decreases to maintain total glomerular filtration rate (GFR), the GFR of the remaining normal nephrons increases. This process is complemented by vasoconstriction of the efferent glomerular arterioles, which results in an increase in intraglomerular pressure and, as a consequence, GFR. In addition, as the number of functioning nephrons decreases, there is an increase in blood flow velocity and hyperperfusion of the remaining nephrons.
Despite the fact that these compensatory mechanisms are aimed at maintaining overall GFR, the resulting glomerular hypertension leads to an increased load on the remaining nephrons and an increase in the rate of their destruction. Glomerular hypertension is also accompanied by an increase in the severity of proteinuria. This creates a vicious circle in which there is continuous death of nephrons and deterioration of kidney function (Fig. 2).
Rice. 2. Vicious circle in CKD in cats
Symptoms of end-organ damage secondary to hypertension may be the first signs of disease that owners and veterinarians notice in cats with CKD. These include:
- Hemorrhages or loss of vision in one or both eyes
- Behavior change
- Ataxia
- Cramps (sometimes)
Treatment
Treatment depends on the leading manifestations of kidney disease, its type, and natural manifestations. General trends:
- Maintain adequate water balance . Dehydration makes a sick cat's condition worse. Therefore, they try to make the cat drink more. If this does not work, enteral tubes are inserted, droppers are placed, solutions are fortified, which are administered to cats with chronic renal failure and CKD.
- They try to preserve the cat’s appetite , which suffers from anemia, uremic gastritis, low potassium, and secondary hyperparathyroidism, when the function of parathyroid hormone is disrupted, which disrupts the calcium-phosphorus balance (hyperphosphatemia occurs).
- Prescription of drugs. To avoid complications from uremic gastritis, they try to prescribe drugs such as Omez, antiemetics (in particular the latest generation - Sereniya), as well as unsaturated omega-3 fatty acids, which have anti-inflammatory and antioxidant properties.
- Monitor potassium levels . Especially if it drops below 3.5 mmol/l. Hypokalemia is a very serious condition that can cause vomiting, seizures, and muscle weakness.
- Constantly monitor and regulate the level of phosphorus in the blood with the help of nutrition and phosphate binders. Phosphate binders are drugs that bind phosphorus in the gastrointestinal tract. These are aluminum preparations, Almagel, aluminum hydroxide, lanthanum carbonate and Ipoketin, which are also available in the Russian Federation. As far as I know, aluminum hydroxide and lanthanum carbonate are not available in the Russian Federation.
- Regulation of metabolic acidosis and control of blood pressure (hypertension) that accompany proteinuria. In particular, drugs such as Amlodipine, Telmisartan and other ACE inhibitors, as well as drugs from the ARB group, are used.
- Anemia control . With anemia, the endogenous synthesis of erythropoietin (the kidney hormone that controls the formation of red blood cells) decreases, low hemoglobin and hematocrit occur, and uremic toxins impair the integrity of red blood cells. In this regard, it is especially important to provide natural, rich protein nutrition. If this does not help in the terminal stages, Erythropoietin is administered in the form of medications.
Diet therapy
The most important point in the treatment of CKD and chronic renal failure is diet therapy. In this case, the owner is always faced with a choice: use complete food or remain on a natural diet. Here I will resort to data from American scientists such as Lisa Pearson and Karen Becker, who say that cats are meat eaters.
Cats are reluctant to eat medicinal food, especially kidney food. I can say this from my own practice. These foods have low levels of protein and are quite tasteless. No one has canceled the fact that cats are meat eaters, even with CKD and chronic renal failure. Therefore, a natural diet may well be the main diet for cats with CKD, but it needs to be modified in several ways.
- To reduce hyperphosphatemia, you can add eggshells instead of the meat and bone component. It contains calcium, but does not contain phosphorus. Thus, we reduce the proportion of phosphorus from 2% to 0.8%.
- We increase the fat content of the diet: fats reduce the level of phosphorus, preventing it from being absorbed. Some calories from fat enter the body, replacing calories from protein. This way the cat remains strong and does not weaken.
- We enrich our natural diet with salmon and krill oils as sources of omega-3 fatty acids, which are very important in dietary therapy for kidney diseases. The fish itself is not given.
- The food is enriched with B vitamins, which are essential in this case.
Thus, we do not reduce the level of protein in the diet to 20% and do not increase the level of carbohydrates, as is generally the case with dry food. Instead, we create a diet where protein will be 40% instead of 60-70%, and increase the fat content of the diet to 60% of calories.
Lisa Pearson says a low protein diet for cats is bad. With such a diet, they are more likely to die from hypoproteinemia (low protein in the blood) than from hyperazotemia (i.e., from chronic renal failure). This means high-quality, bioavailable protein, equivalent to what cats eat in the wild.
Lisa Pearson also says that you need to maintain adequate water balance. Therefore, it is all the more strange that a cat with kidney failure is prescribed dry food, and liquid is administered subcutaneously or intravenously. This is rather than administering fluids internally through a moisture-rich diet. This creates a paradox: the liquid enters the body in an unnatural way.
To summarize what Lisa Pearson recommends for kidney disease in cats:
- It is advisable to avoid dry food.
- Reduce phosphorus levels in your natural diet.
- Saturate your natural diet with fish oil (omega-3 fatty acids).
Chronic kidney disease has no cure. Because nephrons die, it is a progressive disease. The success of treatment and the longevity of an animal with CKD depends on the stage at which it is diagnosed. The sooner this happens, the more successful the treatment will be. If you notice that something is wrong with your cat, you need to consult a doctor and conduct a comprehensive examination of the animal.
Your veterinarian Natalia
? If you are a SUPERPET client, you can sign up for a consultation with Natalia for free in your personal account on the website (or write to the support team in the chat).
Renin-angiotensin-aldosterone system (RAAS) and CKD
The renin-angiotensin-aldosterone system, or RAAS, is a sequence of hormonal reactions aimed at maintaining blood pressure within a narrow normal range. Strict blood pressure control is achieved by maintaining a balance between the following processes:
- Vasoconstriction
- Vasodilation
- Control of extracellular fluid volume and blood volume by excretion or retention of sodium and water.
Angiotensin II is the active end product of a cascade of hormonal reactions. It binds to angiotensin II receptors on the surface of cells in various tissues and causes various biological effects, which are depicted in Fig. 3.
Rice. 3. Renin-angiotensin-aldosterone system (RAAS) and its effect on homeostasis
Types of disease
Highlight:
- Unilateral hydronephrosis
- Bilateral hydronephrosis
In the first case, the pyelocaliceal complex is affected only on one side, in the second - on both sides. Unilateral damage usually occurs against the background of congenital narrowing, conflict with abnormal renal vessels, as well as urolithiasis. The cause of a bilateral process can be stones, tumors or prostate adenoma.
The doctor knows how to treat kidney hydronephrosis at one stage or another. It is only important for the patient to contact a specialist as soon as possible.
Clinical manifestations of CKD in cats
Cats with CKD exhibit a wide variety of nonspecific clinical manifestations. It is important to remember that the clinical manifestations of CKD are related to loss of renal function and not to damage to the kidneys themselves.11-13
The most common clinical manifestations of CKD in cats are:
- Primary polyuria (PU)
- Compensatory polydipsia (CP)
- Lack of appetite
- Weight loss
- Lethargy
Other clinical manifestations include gastrointestinal symptoms such as intermittent vomiting, constipation and halitosis.
Diagnosis and treatment of renal failure in cats
Your veterinarian will do blood and urine tests. X-rays, an ultrasound (an image of your cat's insides), or a biopsy (a tissue sample) may also be needed to make a diagnosis.
If kidney disease is found, treatment can range from surgery to remove the blockage and intravenous fluids to a special diet and medications. You can also inject the liquid under your cat's skin at home.
Talk to your veterinarian about the best options. The kidney diet is low in phosphorus and protein and enriched with vitamin D and omega-3 fatty acids.
Remember that it is important to gradually introduce your cat to new food. Your veterinarian will be able to advise you on how to make this transition easier. With a carefully observed diet. With plenty of clean, fresh water, a serene environment, and regular checkups, you can help your cat live the best life possible.
Prognosis of CKD in cats
As a rule, CKD in cats is characterized by a slowly progressive course and irreversible degenerative processes; This pathology has a high level of morbidity and mortality. If left untreated, CKD is a common cause of death or euthanasia in cats.19
Rice. 4. Cats with mild to moderate CKD die from kidney failure in 57% of cases. 19;
CKD = chronic kidney disease; CVD = cardiovascular disease
Renal obstruction (ureteral obstruction with hydronephrosis)
Kidney stones can fragment and travel through urine into the ureter, the long, narrow tube that connects each kidney to the bladder. They are likely to cause severe pain as they move, and significant difficulty in functioning results in the kidney if they become lodged in the ureter, causing partial or complete blockage. New urine cannot pass out of the kidney easily and it recedes, causing the kidneys to swell. If there is enough pressure, the kidneys become enlarged (hydronephrosis) and damaged. If both ureters become blocked at the same time, this can lead to catastrophic consequences, including death.
Anamnesis
Typically, CKD is found in cats over 6-7 years of age2 and is most common in cats over 10 years of age (>35%).22 The following clinical manifestations occur:
- polyuria
- polydipsia
- anorexia
- loss of appetite
- vomit
- weight loss
- lethargy
- halitosis (bad breath)
In some cases, the first signs of the disease are manifestations of hypertension, such as vision loss or ataxia.
Types of kidney failure
Depending on the course of the disease and its external manifestations, there are:
- Acute form – acute renal failure (ARF);
- The chronic form is chronic renal failure (CRF).
Both forms have similar characteristics, but develop differently.
Acute form
ARF develops very quickly. The signs of the disease are clearly expressed, which allows you to start treatment at an early stage, and this is extremely important for restoring kidney function.
The acute form has three types:
- Prerenal - the volume of circulating blood through the kidneys decreases, but the organ tissues are not damaged, this is the first stage of acute renal failure;
- Renal – renal tissues and structures are damaged;
- Postrenal - caused by mechanical blockage or compression of the urinary organs - ureter, bladder, urethra.
If acute renal failure occurs periodically, then the cat may develop a chronic stage, which cannot be treated.
Chronic form
Chronic failure is accompanied by the death and aging of cells in the kidneys. The number of working cells decreases, and those that remain bear a significantly greater load.
The danger of the chronic form is that at an early stage, when the cat can still be helped, there are no symptoms of the disease. They appear only when more than 2/3 of the kidneys are damaged.
Chronic renal failure occurs in four stages:
- Early stage, in which symptoms are not visible, treatment is not prescribed due to ignorance of the disease;
- Initial stage - the animal already feels slightly unwell, there is a decrease in appetite, slight weight loss, the coat becomes dull;
- Conservative stage – the cat’s health is much worse, the cat’s severe weakness is noticeable, the animal is thirsty, frequent and copious urination occurs, possibly increased blood pressure, diarrhea and vomiting;
- The terminal stage is a severe stage of the disease. Your health is deteriorating more and more, and the smell of acetone may come from your mouth. When performing an ultrasound, bumps are visible on the kidney, the layers are unclear, the kidneys decrease in size.
Analysis of urine
Simultaneous testing of urine and blood samples is an important step in the diagnosis of CKD in cats and is increasingly used in practice in Europe. Among the studied indicators, the most frequently assessed is the relative density of urine (RUD); Some cats with CKD have isosthenuria, with TPR ranging from 1.007 to 1.015.23-25 Urine testing can identify other pathological changes that occur in cats with CKD, such as proteinuria or concomitant urinary tract infection (UTI).
Infection of the kidney tissue (pyelonephritis)
Infection of kidney tissue by bacteria or, less commonly, fungal organisms is one of the kidney diseases that may have a more favorable outcome, so your veterinarian will be on the lookout. Our goal when treating pyelonephritis is to kill the bacteria that cause destructive inflammation. This should limit the progression of any chronic kidney disease or aid in recovery from acute kidney injury. Urine bacterial culture and susceptibility can determine the type of infection and determine which antibiotic may work best.
A new era in the treatment of CKD in cats
The relevance of RAAS blockade in the treatment of CKD.
Typically, medications that block the effects of the RAAS are used to treat CKD in cats. As a result of blockade of the RAAS, there is a predominant expansion of the efferent glomerular arterioles, a decrease in intraglomerular pressure and, as a consequence, a decrease in the severity of proteinuria. Reducing proteinuria in cats with CKD is important because:
- Even with low protein concentrations, proteinuria is a poor prognostic sign for survival in feline CKD 28,29
- As the severity of proteinuria increases, the risk of death increases26
Other undesirable effects of angiotensin II and aldosterone (on the heart and kidneys) can also be reduced by blocking the RAAS.30-34
Angiotensin receptor blockers (ARBs) are a new class of pharmaceutical drugs for veterinary use developed to reverse the adverse effects of angiotensin II and aldosterone.
What are angiotensin receptor blockers (ARBs)? Angiotensin receptor antagonists or blockers (ARBs) are a class of molecules that directly bind to angiotensin II receptors, in contrast to angiotensin-converting enzyme inhibitors (ACEIs), which block the angiotensin-converting enzyme (ACE) (Figure 6).
Rice. 6. Diagram illustrating the targeted mechanism of action of ARBs
There are two main types of angiotensin II receptors: AT1 and AT2. Most of the functions of angiotensin II are mediated by AT1 receptors.35 These receptors are found in the blood vessels, kidneys, liver, heart, adrenal gland and pituitary gland. AT2 receptors appear to slow the body's response to angiotensin II, and many of the effects of AT2 receptors are opposite to those of AT1 receptors.
Reasons for development
The following factors can lead to the development of pathology:
- Congenital anomalies. These include incorrect location of the ureter or its entry into the bladder, as well as the arteries of the kidneys and their branches
- Inflammatory processes in the bladder and ureter
- Urolithiasis disease
- Tumor-like formations in the pelvis
Call now
(495) 7 800 500
Leave a request
You will receive an automatic call back, wait for the operator to respond.
* By clicking the “Order a call” button, you agree to the processing of your personal data by JSC Group
Policy regarding the processing of personal data Consent to the processing of personal data
Make an appointment
How are ARBs different from ACEIs?
Due to their targeting of specific receptors18,36,37, ARBs have two obvious advantages over ACEIs :
1) targeted mechanism of action: the effect is directed only at AT1 receptors, through which most of the adverse effects of angiotensin II are mediated in conditions of impaired renal function (Fig. 7). The beneficial effects of AT2 receptor activation are maintained.35
Rice. 7. Diagram illustrating the benefits of selective blockade of AT1 receptors
2) ARBs such as telmisartan (Semintra®) directly and selectively block AT1 receptors and do not inhibit ACE.35 In response to inhibition of enzymatic activity during the hormonal cascade, the necessary enzymes are bypassed. In response to inhibition of ACE, which originates from the renin-angiotensin-aldosterone system, the formation of “tissue ACE” increases, which catalyzes the synthesis of angiotensin II, despite the maximum suppression of ACE. This phenomenon is known as “ACE escape” and has been observed in many mammalian species with long-term use of ACE inhibitors35 (Figure 8).
Rice. 8. Schematic representation of the phenomenon of “ACE escape”
This phenomenon is also typical for cats receiving ACE inhibitors (for example, for the treatment of heart disease).18,38-41 When using ARBs, “ACE escape” does not occur; the clinical results of drugs in this group are associated with a direct effect on AT1 receptors and with the blockade of adverse effects of angiotensin II.
Main symptoms
Most patients complain of the following manifestations of hydronephrosis:
- severe pain in the lower back and abdomen, which can radiate to other parts of the body
- increase in body temperature
- weakness
- chills
- the appearance of blood clots in the urine
- headaches and increased blood pressure
- there may be a completely asymptomatic course when the pathology is present from birth and the body has adapted to it
The more advanced the disease, the more pronounced its symptoms become.
The more advanced the disease, the more pronounced its symptoms become.
Important! Body temperature rises when the disease is accompanied by an infection. In this case, it is very important to carry out immediate treatment.
Symptoms of hydronephrosis may also include bloating, constant nausea and severe vomiting, increased fatigue with decreased performance.
In children, signs of the disease include:
- cloudy urine
- reducing the amount of daily urine
- pain
Like adults, children complain of weakness, headaches, and nausea. Parents should pay close attention to the child’s health if he refuses his favorite food, games, walks, becomes lethargic and sleeps a lot.
Competent treatment of kidney hydronephrosis in an adult or child is impossible without a high-quality comprehensive examination.
Semintra for the treatment of CKD in cats
Semintra® (active ingredient: telmisartan) is the first angiotensin receptor blocker (ARB) registered for use in veterinary medicine*.
(*State register of veterinary medicines as of 03/01/2018)
The drug is specially designed for use in cats:
- Semintra® is designed to reduce proteinuria in chronic kidney disease (CKD) in cats36
- Semintra® contains the active molecule telmisartan, an angiotensin receptor blocker (ARB), and has a targeted mechanism of action
- in most cases, Semintra® in the form of an oral solution was well accepted.37,42
Find out more about Semintra
References: 1. Brown, S. (2005) Urinary System. In: Kahn, C. (ed). The Merck Veterinary Manual. Whitehouse Station: MERCK & CO., INC. 1267-1272. 2. Brown, S. (2007) Management of chronic kidney disease. In: Elliott, J. and Grauer, G. BSAVA Manual of Canine and Feline Nephrology and Urology. 2nd ed. Gloucester: British Small Animal Veterinary Association. 223-230. 3. Brown, S. (2012) “Managing Chronic Kidney Disease (CKD): 10 Common Questions,” Proceedings of the 83rd Florida Veterinary Medical Association (FVMA) Conference, Tampa, FL, May 4-6, 2012. 4. Krawiec , D. and Gelberg, H. (1989) Chronic renal disease in cats. In: Current Veterinary Therapy X. ed. Kirk, R. Philadelphia: W. B. Saunders. 1170-1173. 5. Polzin, D. and Osborn, C. (1986) Update: conservative medical management of chronic renal failure In: Kirk RW, ed. Current Veterinary Therapy IX, Philadelphia: W. B. Saunders. 1167-1173. 6. Boyd, L.M. Langston, C. Thompson, K. et al. (2008) Survival in cats with naturally occurring chronic kidney disease (2000-2002). J Vet Intern Med; 22:1111–1117. 7. Watson, AD (2001) Indicators of renal insufficiency in dogs and cats presented at a veterinary teaching hospital. Aust Vet Practit 31:54–58. 8. Lund, E.M. Armstrong, P.J. Kirk, CA. (1999) Health status and population characteristics of dogs and cats examined at private veterinary practices in the United States. J Am Vet Med Assoc 214:1336–1341. 9. European Pet Food Industry Federation (FEDIAF) (2010) Facts and Figures, FEDIAF, Brussels. 10. Chakrabarti, S. Syme, H.M. Brown CA. et al. (2013) Histomorphometry of Feline Chronic Kidney Disease and Correlation With Markers of Renal Dysfunction. Vet Pathol.50(1):147-155. 11. Polzin, D. (2010) Chronic Kidney Disease. In: Ettinger, S. and Feldman, E. Textbook of Veterinary Internal Medicine. 6th ed. St. Louis: Saunders. 1991-2021. 12. Polzin, D. (2011) Chronic Kidney Disease. In: Bartges, J. and Polzin, D. Nephrology and Urology of Small Animals. Ames: Wiley-Blackwell. 433-471. 13. Maddison, J and Syme, H. (2010) Chronic kidney disease in dogs and cats: Pathophysiology and diagnosis. Irish Veterinary Journal. 63 (1): 44-50. 14. Chetboul, V. Lefebvre, H. Pinhas, C. et al. (2003) Spontaneous Feline Hypertension: Clinical and Echocardiographic Abnormalities, and Survival Rate. J Vet Intern Med. 17:89-95. 15. Snyder, P. Sadek, D. and Jones, G. (2001) Effect of amlodipine on echocardiographic variables in cats with systemic hypertension. J Vet Intern Med. 15: 52-56. 16. Maggio, F. DeFrancesco, T. Atkins, C. et al. (2000) Ocular lesions associated with systemic hypertension in cats: 69 cases. J Am Vet Med Assoc. 217: 695-702. 17. Littman, M. (1994) Spontaneous hypertension in 24 cats. J Vet Intern Med. 8: 79-86. 18. Ruilope, L.M. (2005) Renin-Angiotensin-Aldosterone System blockade and renal protection; antiotensin-converting enzyme inhibitors or angiotensin II receptor blockers? ACTA Diabetol.42:33–41. 19. Elliott, J. Rawlings, J. Markwell, P. et al. (2000) Survival of cats with naturally occurring chronic renal failure: effect of dietary management. J Small Anim Pract; 41(6):235-42. 20. Grauer, G. F. (1998) Urinary tract disorders. In: Nelson RW and Couto CG (eds). Small Animal Internal Medicine. 2nd ed. St. Louis, Missouri: Mosby Inc., pp. 571-670. 21. Bartges, J.W. (2012) Chronic kidney disease in dogs and cats. Vet Clin North Am Small Anim Pract; 42: 669-692. 22. Cooke, K. (2012) “Feline Chronic Renal Failure,” Proceedings of the 83rd Florida Veterinary Medical Association (FVMA) Conference, Tampa, FL, May 4-6, 2012. 23. Acierno, M. and Senior, D. (2010) “Urinary Disorders” In: Schaer, M. Clinical Medicine of the Dog and Cat. 2nd ed. Manson Publishing Ltd. London, 505-561. 24. DiBartola SP. Rutgers H.C. Zack, P.M. et al. (1987) Clinicopathologic findings associated with chronic renal disease in cats: 74 cases (1973-1984). J Am Vet Med Assoc; 9: 1196-1202. 25. Elliott, J. and Barber, P.I. (1998) Feline chronic renal failure: clinical findings in 80 cases diagnosed between 1992 and 1995. J Small Anim Pract. 39: 78-85. 26. Syme, H.M. and Elliott, J. (2006) Proteinuria in Chronic Kidney Disease in Cats- Prognostic Marker or Therapeutic Target. J Vet Intern Med. 20:1052-1053. 27. Paepe, D. Daminet, S. (2013) Feline Chronic Kidney Disease - Diagnosis, Staging and Screening. J Fel Med Surg. In Press. 28. Syme, H.M. Markwell, P.I. Pfeiffer, D. et al. (2006) Survival of cats with naturally occurring chronic renal failure is related to the severity of proteinuria. J Vet Intern Med; 20: 528-535. 29. Brown, SA. Atkins, C. Bagley, R. et al. (2007) Guidelines for the identification, evaluation, and management of systemic hypertension in dogs and cats. J Vet Intern Med; 21: 42-558. 30. Brewster, U. Setaro, J.F. Perazella, MA. (2003) The Renin-Angiotensin-aldosterone system: Cardiorenal effects and implications for renal and cardiovascular disease states. Am J Med Sci;326:15–24. 31. de Paula, R.B. da Silva, A.A. Hall, J.E. (2004) Aldosterone antagonism attenuates obesity-induced hypertension and glomerular hyperfiltration. Hypertension;43:41–47. 32. Panos, J. Michelis, M.F. DeVita, M.V. et al. (2003) Combined converting enzyme inhibition and angiotensin receptor blockade reduce proteinuria greater than converting enzyme inhibition alone: Insights into mechanism. Clin Nephrol;60:13–21. 33. Weir, MR. Dzau, V. J. (1999) The renin-angiotensin-aldosterone system: A specific target for hypertension management. Am J Hypertens;12:205S–213S. 34. Zhou, X. Ono, H. Ono, Y. et al. (2004) Aldosterone antagonism ameliorates proteinuria and nephrosclerosis independent of glomerular dynamics in the L-NAME/SHR model. Am J Nephrol;24:242–249. 35 Dinh, D.T. Frauman, A.G. Johnston, CI. et al. (2001) Angiotensin receptors: distribution, signaling and function. Clin Sci 100:481–492. 36. Semintra Summary of Product Characteristics. 37. CVMP Assessment Report for Semintra (EPAR). 38. Coté, E. MacDonald, KA. Meurs, K. M. et al. (2011) Hypertrophic Cardiomyopathy. In: Feline Cardiology, 1st ed. Chichester: Wiley-Blackwell. 103-175. 39. Aramaki, Y. Uechi, M. Takase, K. (2003) Angiotensin Converting Enzyme and Chymase Activity in the Feline Heart and Serum. J. Vet. Med. Sci. 65(10): 1115-1118. 40. MacDonald, KA. Kittleson, MD. Larson, R.F. et al. (2006) The effect of ramipril on left ventricular mass, myocardial fibrosis, diastolic function, and plasma neurohormones in Maine coon cats with familial hypertrophic cardiomyopathy without heart failure. J Vet Intern Med;20:1093–1105. 41. Akasu, M. Urata, H. Kinoshita, A. (1998) Differences in Tissue Angiotensin II Forming Pathways by Species and Organs In Vitro. Hypertension. 32:514-520. 42. Sent, U. Lang, I. Moore, G. (2013) “Characterization of Telmisartan in Cats”, Proceedings of the ISFM World Feline Veterinary Congress, Barcelona, June 26-30, 2013. 43. Ruilope, L.M. Redon, J. Schmieder, R. (2007) Cardiovascular risk reduction by reversing endothelial dysfunction: ARBs, ACE inhibitors, or both? Expectations from the On Target Trial Programme, Vascular Health and Risk Management 3(1):1–9. 44. Polzin, D. (2013) Evidence-based step-wise approach to managing chronic kidney disease in dogs and cats. J Vet Em Crit Care; 23(2):205-215. 45. Westfall, D. Twedt, D. Steyn, P. et al. (2001) Evaluation of esophageal transit of tablets and capsules in 30 cats. J Vet Intern Med; 15:467–470. 46. Ebner, T. Schaenzle, G. Weber, W. (2012) In vitro glucuronidation of the angiotensin II receptor antagonist telmisartan in the cat: a comparison with other species. J. Vet Pharmacol. Therap 36: 154–160. 47. Bradshaw, J.W. Goodwin, D. Legrand-Defrétin, V. et al. (1996) Food selection by the domestic cat, an obligate carnivore. Comparative Biochemistry and Physiology Part A: Physiology. 114(3), p205-209. 48. Sparkes, A.H. Helene, R. Lascelles, D.B. (2010) ISFM and AAFP Consensus Guidelines: Long-term use of NSAIDs in cats. J Fel Med Surg 12:521–538. 49. Caney, S. (2011) Caring for a cat with chronic kidney disease. 2nd ed. Vet Professionals. London. 50. Elliott, J. and Elliott, D. (2008) Nutritional management of feline chronic kidney disease. Veterinary Focus. 18(2):39-44.
Diagnostics
Competent treatment of kidney hydronephrosis in an adult or child is impossible without a high-quality comprehensive examination. Only it allows you to determine the type of disease, the degree of organ damage and other features of the pathology.
Diagnostics include:
- clinical and biochemical blood tests
- Analysis of urine
- Kidney ultrasound
- X-ray examination of the kidneys
- CT and MRI
- cystourethrography
- radioisotope study (nephroscintigraphy)
Treatment methods
Therapy should be started as early as possible. It can be carried out by two main methods: medication and surgery. The choice of technique is made exclusively by the doctor. In this case, the specialist takes into account a number of factors, including: the degree of development of the disease, the functionality of the organ, age and other individual characteristics of the patient, the cause of hydronephrosis, etc.
Call now
(495) 7 800 500
Leave a request
You will receive an automatic call back, wait for the operator to respond.
* By clicking the “Order a call” button, you agree to the processing of your personal data by JSC Group
Policy regarding the processing of personal data Consent to the processing of personal data
Make an appointment
Conservative therapy
This treatment is aimed at eliminating pain, as well as fighting infection and preventing complications. It is very important to prevent the development of urolithiasis and kidney failure.
Doctors can prescribe drugs from the following groups:
- antibacterial
- uroseptic
- anti-inflammatory
Important! It should be understood that in most cases, conservative therapy does not get rid of the cause of the disease. It is aimed only at eliminating symptoms and does not allow the pathology to become chronic.
Therapy should be started as early as possible. It can be carried out by two main methods: medication and surgery.
Surgical interventions
Operations are performed to ensure normal urine flow and kidney function.
In case of serious disorders caused by obstructed urine outflow, the following is carried out:
- Stenting.
A stent, which is a flexible and thin tube, is placed in the ureter. It ensures the free flow of urine from the kidney to the bladder. The tube begins in the pelvis area and ends in the bladder. The indication for installation of a stent is the need to ensure the outflow of urine when the urinary tract is blocked. The stent is removed immediately after the cause of the blockage is eliminated - Nephrostomia.
This intervention involves a whole range of surgical techniques. The procedure is temporary and precedes a full-fledged surgical operation to eliminate hydronephrosis. When intervening in the area of the renal pelvis, drainage is inserted in the form of a catheter. The outer end of the catheter is connected to a urinal
Important! Both of these measures are temporary. They only ensure normal urine flow, but do not cope with the cause of hydronephrosis.
The pathology is eliminated exclusively by surgery.
Operations are performed to ensure normal urine flow and kidney function.
Today can be held:
- Laparoscopic interventions
- Manipulations using the da Vinci robot
Experienced doctors who know modern working methods try to carry out interventions using minimally invasive methods. This allows you to reduce the risks of various complications and shorten the patient’s rehabilitation period. Particular attention is paid to organ-preserving technologies.
Interventions are aimed at plastic surgery of the pelvis or ureter, removal of tumors, crushing stones or removing them from organs and cavities. If during the examination it is determined that the functioning of the kidney is partially or completely impaired, operations may be performed to remove it.
Important! Even after removal of the kidney, the patient can return to his normal life (with some restrictions in physical activity and nutrition).
Before starting treatment for kidney hydronephrosis in adults and children, an examination is carried out to assess the cause of symptoms, determine the degree of damage and other features of the course of the disease.