Treatment processes for pets often take a considerable amount of time and effort from pet owners. In nature, there are many different diseases that require a lot of time to fight them. By the way, ringworm, a fairly common dermatological disease , characterized by local or general damage to the skin, also falls under this definition. Ringworm in cats, as a rule, appears in the early years of development and formation of the individual. The group of causative agents of this disease includes the fungi Microsporum (microspores) and Trichophyton (trichophytes). In this regard, it is customary to distinguish several different types of lichen. Their main number includes varieties such as microsporia and trichophytosis. We will be able to study in more detail all their main differences and features a little later.
Based on medical research, we can say that ringworm belongs to the category of zoonotic diseases that can be transmitted to humans under certain conditions. That is why it is important to quickly identify and eradicate this disease in your pet. Ringworm in cats in most cases occurs due to :
- young age of the individual;
- genetic characteristics;
- poor nutrition and lack of vitamins;
- decreased immunity;
- concomitant diseases.
Thus, the vast majority of recorded cases indicate the occurrence of fungal diseases exclusively in young individuals with weak immunity. At the same time, the deterioration of the pet’s general condition in this case can be provoked by both natural and artificial factors - infectious diseases, lack of minerals and vitamins, potent drug therapy. In addition, it is worth noting the obvious predisposition to infection in eastern breeds (Persians, exotics). But how does the process of developing such an unpleasant disease occur? The initial progression of lichen is mainly caused by the appearance of a fungal vector.
What is microsporia in cats: information about pathology
Microsporia in cats is a separate fungal pathology, usually caused by a fungus of the species Microsporum Gypseum, sometimes by other representatives of the genus Microsporum. The problem is that in practice all pathologies caused by pathogens from the genus Trichophyton are also called the same.
In fact, they cause a separate disease called trichophytosis. To the eye (and in many other ways), the differences between these two diseases are so minimal that in practice, veterinarians usually call all these diseases dermatophytes, without making any special distinctions between them.
There is one more important nuance concerning the same Microsporum Gypseum. Scientists are still arguing about its exact species specificity, but there is little sense in this: it is known for sure that this parasitic fungus can affect not only cats, but also dogs, chinchillas, rabbits, other domestic and wild animals, as well as humans. The worse the potential host’s immunity, the greater the chance of infection.
Interesting! The feline variety of this disease is considered the most unpleasant. The reason is the increased virulence and infectiousness of the cat strain.
For example, the canine strain of the pathogen is not that dangerous for humans (albeit with reservations), although just one contact with a sick cat (which may well not have signs of the disease) results in infection with a probability of about 70%.
Ways of spreading fungal spores
Well, we previously looked at the introductory information that describes the concept of ringworm. In addition, we paid special attention to factors that contribute to rapid infection . But how does the process of disease progression occur? Is it possible to warn yourself and your pet?
Previously, we have already drawn the attention of readers to the sources of damage. Ringworm in cats is formed due to direct contact with fungal spores, characterized by microscopic sizes. It is almost impossible to record the presence of dispute data without any professional equipment. Microsporia, like, strictly speaking, trichophytosis, is rightfully considered an extremely common disease, occurring in both street and domestic animals. Veterinary service specialists currently identify 4 channels of infection:
- direct contact with an affected individual;
- indirect contact through personal objects of the affected individual;
- spread of spores by rodents;
- transfer of fungal pathogens on clothing.
The list presented above clearly demonstrates all the ways spores can spread. It is worth noting that the pathogens themselves are characterized by high resistance to external factors. In this regard, they can be active over a fairly long period of time. Transmission of the disease from cat to human is not recorded so often. In most cases, only preschool children and adults who, due to certain reasons, have weak immunity, are exposed to damage processes. A healthy human body prevents the development of the disease by effectively suppressing the activity of fungal pathogens.
But what to do if an infection occurs? What does ringworm look like in cats and how can it be recognized? We will try to present the results of studying these issues in the next section devoted to the symptoms of the disease.
Basic differences between microsporia and trichophytosis
As we have already written, the differences between microsporia and trichophytosis are small, but they still exist:
- With microsporia, the parasite lives on the surface of the hair, while with trichophytosis it affects the hairs from the inside.
- Microsporia can usually be diagnosed using a Wood's lamp, while fungi of the genus Trichophyton usually do not reveal themselves under UV radiation.
- Unlike trichophytosis, microsporia is usually accompanied by quite severe itching.
It should be noted that the differences listed above are not very specific, and in practice the difference between diseases becomes even more blurred. The only 100% difference is the location of the pathogen (on the fur/inside the hair).
Symptoms, initial stage and first signs of microsporia in cats
Owners need to remember that the symptoms, initial stage and first signs directly depend on what particular form of microsporia their pet has developed.
But it is still possible to identify the main symptoms, which are typical for all forms of the disease:
- A sudden and inexplicable change in the condition of the cat's fur. With microsporia, it can become rarer, stiffer, brittle and unpleasant to the touch.
- You can see a grayish coating on your pet's fur. True, this only works in the case of light-colored cats, as well as completely black pets.
- The cat becomes restless and itches often.
- Bald patches on a cat's body. In mild cases or in the early stages, they usually appear on the face, ears, chin, as well as on the abdomen and genital area.
- The skin of a sick cat begins to peel off and even become scaly.
- There are no signs of severe inflammation in the bald areas, but they gradually grow. If you look closely, the skin in these places is literally strewn with “stumps” of hair broken off at the root.
- If left untreated, the cat becomes completely bald, covered with scales and scabs, and wounds and ulcers appear on its skin, which are quickly contaminated with pathogenic microflora. Not all cats survive to this state, since the animal usually dies much earlier from sepsis or secondary infections.
Surface form
The easiest and most common option. In this case, bald patches with hair stumps quickly appear on the cat’s skin. As a rule, the process develops quite quickly, within a maximum of three weeks.
Very often, the skin of a sick cat is infested with pathogenic microflora, which is why pyoderma and other variants of purulent inflammation of the skin are not uncommon.
Deep, follicular microsporia
The most severe version of the disease. Fortunately, it doesn't happen often. But if the symptoms described below appear, the owner needs to urgently take the cat to the nearest clinic:
- Bald patches quickly appear on the skin.
- On bald areas of the skin, ulcers, scabs, and deep wounds form in just as short a time. All these injuries do not heal, but quickly fester.
- Damage has an unpleasant tendency to merge and form peculiar conglomerates. The general condition of the cat quickly deteriorates, and the pet is at great risk of dying due to sepsis.
Hidden microsporia
In cats, this variant is found only slightly less frequently than the superficial form. Microsporia in this variant is extremely insidious, since for a long time the cat does not have any clear clinical signs, but at the same time it is already contagious both to other animals and to humans.
However, with luck and some attention, you can see signs that something is wrong:
- Grayish coating on the fur.
- The animal scratches itself frequently, even if it is wearing antiparasitic collars.
Clinical manifestations characteristic of microsporia can take a long time to develop, sometimes over several months. In addition, this variety often becomes chronic, characterized by periodic relapses.
Erased form
The rarest variety. In fact, in this case the disease is chronic, relapses manifest as the formation of small bald patches and crusts on the pet’s skin. As a rule, there are no other clinical signs.
Of course, in this case too, the pet is contagious to surrounding animals and people.
MICROSPORIA Article magazine “Attending Physician” 04.01
MICROSPORIA
Article in the journal “Attending Physician” 04.01
V.M.Rukavishnikova, KMN
Modern features of the clinic and treatment of MICROSPORIA
What are the sources and routes of transmission of microsporia? What is the clinical picture of typical microsporia and its atypical forms? What is the rational therapy for microsporia?
Zooanthroponotic microsporia is the most common highly contagious disease of the skin and hair, common to humans and animals.
It is characterized by damage to coarse hair of the head, upper lip, chin, eyebrows, eyelashes, pubis, labia, as well as vellus hair of smooth skin. The causative agents of microsporia are zoophilic, anthropophilic and geophilic fungi of the genus Microsporum. Of the more than 20 species of this fungus, the most important in human pathology is the zoophilic fungus - fluffy microsporum. This is a kind of cosmopolitan fungus, practically the only causative agent of microsporia in the world, with the exception of African countries.
Microsporia predominates in European countries, especially in the Mediterranean, the USA and South America, Japan, Israel, Kuwait, Qatar, and the United Arab Emirates [1, 3, 5, 7, 9].
Today, microsporia has become most widespread even in regions with a traditionally high incidence of trichophytosis. Thus, in Dagestan, Uzbekistan, Tajikistan, Turkmenistan, Bashkortostan, Kazakhstan, Armenia, where isolated cases of microsporia were previously observed, today it accounts for up to 83–99.7% of all fungal hair diseases [3, 5].
In Russia, the incidence of microsporia is about 71.6 per 100 thousand population. In Moscow and the Moscow region it accounts for 96.2% of all dermafitia with hair damage [3].
Microsporia mainly (up to 65%) affects children, including newborns.
The main source of infection (80.5%) are cats, mainly stray ones. Cats living in medical institutions pose a particular danger, as they infect sick patients. However, cats sold at the Bird Market, near Durov’s Corner, as well as in pet stores and special clubs can also be dangerous, although they are equipped with special certificates, and some of them are even vaccinated. We witnessed how an expensive, elite breed of cat, distinguished by its particularly beautiful shape and color, became a source of infection for three generations in a family. Given to her granddaughter for her birthday, it infected her grandparents, the hero of the occasion, as well as her parents.
In most cats, which serve as a source of infection, foci of microsporia are determined clinically in the form of areas of baldness on the skin of the face, around the mouth and nose, on the outer surfaces of the ears, front and hind legs, and on the tail. The skin in areas of baldness appears flaky with the presence of unevenly broken hair, and sometimes new hair growth is observed in the center of such areas. Under a Wood's lamp, the green glow of the affected hair, characteristic of microsporia, is determined.
In another group of cats, lesions may not be visible to the eye, but are detected during fluorescent examination. Finally, in approximately 2–2.4% of cats, the lesions are not visible to the eye and are not detected under a Wood's lamp, but when combed from their hair, a culture of fluffy microsporum can be obtained.
Although one of the synonyms for fluffy microsporum is microsporum canis (canine), dogs appear as a source of infection in only 4% of patients with microsporia.
Rare animals that suffer from microsporia and can become a source of infection for people include monkeys, tigers, lions, wild and domestic pigs (especially piglets), horses, sheep, silver-black foxes, rabbits, rats, mice, hamsters, guinea pigs and other small rodents, as well as birds - pigeons, crows, chickens, which are hunted by sick cats. Animals become infected from the cats themselves or from their fur falling on plants, straw, or grain. In addition, fluffy microsporum can be carried on their legs by domestic insects, in particular cockroaches.
In 5.5% of patients with microsporia, the sources of infection are people - relatives, friends, neighbors - if basic sanitary and hygienic rules are not observed, as well as sexual partners when foci of mycosis are localized on the external genitalia, pubis, abdomen, upper thighs.
Homeless people and beggars, in addition to lice and scabies, can become carriers of fungal diseases.
Household items - a stroller left overnight in the entrance and favored by cats, toys, combs, underwear, etc. become a source of infection in 2-2.5% of patients with microsporia.
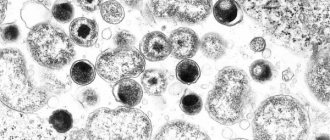
| Figure 1. Microsporia of smooth skin |
The incidence of microsporia varies throughout the year and largely depends on the appearance in cats, which are the main source of infection, of kittens that are more susceptible to infection and microsporia. Although pregnancy in cats lasts seven weeks and offspring appear several times a year, two outbreaks of microsporia disease in humans can be identified. The first occurs in May-June and is associated not only with the birth of kittens that are attractive to children, but also with greater freedom for children in the summer, their greater contact with the animal world when moving to the village, to the country, to health, sports and labor camps. Another increase in incidence is observed in September - November, when children return to the city and are carefully examined not only by their parents, but also by health workers when they enter schools and kindergartens. In this case, both fresh and erased, previously unrecognized forms of microsporia are identified [3].
| Figure 2. Disseminated foci of microsporia |
The incubation period for microsporia is usually five to seven days. After it, on smooth skin, mainly on open areas of the face, neck, chest, upper and lower extremities, single (from one to three) round-oval erythematosquamous spots 1–4 cm in diameter, clearly outlined by a peripheral ridge, appear (Fig. 1 ). If the kitten is warmed under a shirt, taken to bed, and the primary foci of mycosis are rubbed while washing with a washcloth, multifocal, disseminated variants of microsporia arise (Fig. 2). The spread and fusion of mycosis foci is also facilitated by irrational treatment, in particular lubrication with corticosteroid creams.
| Figure 3. Foci of microsporia with “stumps” of hair wrapped in sheaths |
Typical foci of microsporia on the head are usually located on the crown, in the parietal and temporal regions. They look like round-oval “bald patches” up to 3–5 cm in diameter with clear boundaries and “screenings” near them. The hair in the lesions is dull, all broken off at the same level, at a height of 4–6 mm, as if trimmed. Apparently, this is why microsporia is called “ringworm” in everyday life. The surface of the focus of mycosis appears rough, shagreen due to protruding “stumps” of hair, shrouded in grayish or whitish sheaths (Fig. 3). Under a Wood's lamp, the affected hair glows bright green, resembling a freshly mown meadow.
Microsporia is traditionally considered a disease of childhood. However, nowadays adults are also often affected by this mycosis. Apparently, unfavorable social and environmental conditions, an increase in neuroendocrine diseases and immunodeficiency conditions have an effect. If in 1932 A. M. Arievich observed microsporia in 6 adults out of 6000 patients, now adults account for up to 35% of cases of the disease. Women get sick four times more often than men.
In children, microsporia, as a rule, is diagnosed in a timely manner; atypical forms and errors in diagnosis are observed in 5% of cases; in adults, this figure increases almost four times and amounts to 19% of cases [3].
Of the atypical forms of microsporia, erased, trichophytoid varieties deserve special attention. They are not so rare: in 8.5% of patients, and in adults 2.5 times more often. Such microsporia occurs unnoticed, hardly bothers patients and does not force them to immediately consult a doctor. It is often confused with seboreids, seborrheic dermatitis, psoriasis and other diseases, and incorrectly selected treatment does not bring results. In this regard, such variants of microsporia become chronic, becoming the cause of further dissemination of mycosis in the sick person and its spread in the environment. The duration of trichophytoid microsporia has been recorded from seven months to two years.
Such forms of microsporia are usually characteristic of aggravated patients (tuberculosis, Sjögren's disease, pellagroid dermatitis, etc.). Clinically, they are manifested by diffuse or focal peeling, sparse hair, or the formation of areas of focal alopecia. The hair in the lesions is dull, without covers, broken off in different ways - at the level of the skin and at a height of 10–15 mm. Areas of alopecia are either very small, about the size of a pinhead, or gigantic, polycyclic in shape when merging.
On smooth skin, foci of microsporia appear as low-inflammatory, slightly flaky or depigmented round-oval spots. When they merge, polycyclic foci of mycosis may appear, blurred, indistinct, without clear boundaries, slightly itchy. In one of our patients, a 69-year-old cat lover, trichophytoid microsporia of the scalp was not diagnosed for two years. In the past, she suffered from tuberculous lymphadenitis and mesodenitis and took maintenance doses of prednisolone for a long time (for 10 years) for Shagren's syndrome. Microsporia was manifested in her by peeling of the scalp, hair loss, mainly in the occipital region, and itching. All phenomena intensified in the warm season and subsided in the cold season. The disease was treated for a long time and unsuccessfully with drugs used for seborrheic dermatitis or psoriasis. The diagnosis of microsporia was helped by the appearance of fresh typical foci of mycosis on the skin of the face and neck. When the patient was shaved, it turned out that almost the entire scalp was involved in the pathological process. An identical culture of fluffy microsporum was obtained from all foci of mycosis on the head, face, neck, as well as from squamous-keratotic rashes on the skin of the palms.
Sometimes an unusual source of infection also misleads the doctor, and microsporia may not be diagnosed even in children, which leads to the trichophytoid form. Thus, an eight-year-old girl fell ill after a week of contact with a sick pigeon, which she and her father had captured from a cat apparently suffering from this mycosis. While nursing the pigeon, the girl took it in her arms, swaddled it, and fed it. A clearly defined spot appeared on the top of the child’s head, covered with silvery scales. The hair in the lesion was not broken off, there were no subjective sensations.
The girl was diagnosed with psoriasis and was treated with diprosalic and ditrastic. During this time, the skin process spread to the entire scalp and became complicated by folliculitis and perifolliculitis. The changes were regarded as a complication of psoriasis by secondary pyococcal flora, and therapy was supplemented with antibiotics - geoxizone and fucarcin. The child's condition kept getting worse. Hair fell out in large quantities, and the girl experienced pain when combing it. With a presumptive diagnosis of discoid lupus erythematosus, the patient was referred to the Central Clinical Hospital.
A detailed examination revealed diffuse peeling of the entire scalp, sparse hair, atrophic bald patches, which were especially numerous in the parietal-occipital region. In some places the peeling was insignificant, but areas of scar atrophy of various sizes and shapes were clearly defined, without clear boundaries, almost without inflammatory phenomena. Near the scarred skin, the hair fell out easily, was dull, thinned, curled, and refracted light unevenly. The length of the hair was maintained or it broke off either at skin level or at a height of 10–15 mm. Scraping the skin in the lesions was painful. After removing the scaly crusts, the skin appeared moist and inflamed. After shaving and washing, it turned out that the entire surface of the head was covered with multiple lesions (more than 60), some of them were the size of a lentil grain, others were 2-3 cm in diameter, there were also giant areas of 8x12 cm. Enlarged and painful posterior cervical and parotid lymph nodes. Microscopically, clusters of small spores were detected on the surface of the affected hair. Under Wood's lamp, a not entirely characteristic grayish-whitish glow was detected. However, a typical culture of fluffy microsporum was obtained on a nutrient medium. Thus, late diagnosis and inadequate treatment led to the fact that the focus of superficial microsporia, which usually passes without any consequences, was complicated by the dissemination of the fungal process throughout the entire scalp, the formation of areas of cicatricial atrophy and focal alopecia, and lymphadenitis.
Perhaps, deep - infiltrative-suppurative, kerion-like or granulomatous variants of microsporia with pronounced symptoms deserve even more attention and alertness. They are recorded in 4.5–6.5% of patients with this mycosis. They are characterized by severe disease, pain, fever and other symptoms of intoxication. The course of the disease is complicated by lymphadenitis and allergic rashes, with a rapid outcome in cicatricial atrophy and irreversible focal alopecia.
As a rule, deep forms of microsporia occur in weakened children or adults, mainly in women with endocrine or immune pathologies (dysfunction of the reproductive and thyroid glands, pituitary dwarfism, lymphogranulomatosis, blood diseases). Sometimes superficial variants of microsporia are transformed into infiltrative-suppurative ones under the influence of inadequate treatment, as well as repeated injuries, including with a washcloth during washing and going to steam rooms. This is facilitated by frequent sea bathing, and most importantly, constant stay in a damp, tight-fitting bathing suit.
In adults, foci of deep microsporia are usually detected on the skin of the legs or pubis and labia, in children - on the scalp.
Kerion-like foci of mycosis appear to be large, confluent, occupying large areas of the scalp or the entire area of the pubis and outer labia. This is usually a conglomerate of merged and suppurating painful folliculitis, perifolliculitis and abscess elements. Due to edema, infiltration and impetiginization, microsporia foci rise above the skin level. Their surface is covered with rough purulent crusts with loose and partially melted hair stuck together in them. After removing the crusts and hair from the gaping openings of the hair follicles, a creamy pus is released like honey from a honeycomb (kerion-honeycomb). Regional lymph nodes are enlarged and painful. Such patients are characterized by severe symptoms of intoxication, allergic rashes up to erythema nodosum of the legs. Often, such forms of microsporia are mistaken for ulcerative-vegetative pyoderma, infiltrative-suppurative trichophytosis, psoriasis complicated by pyoderma.
In young girls with hypertrichosis, deep microsporia of the legs may occur, usually mistaken for vasculitis, Majocchi granuloma, reticulosis. In these cases, relatively small (2-3 cm in diameter), deep, single, follicular-nodular lesions are located on the lower leg in the form of a ring.
We present a fairly typical story of the formation of infiltrative-suppurative microsporia in a seven-year-old boy. It all started with the appearance, usual for this mycosis, of a small round patch of baldness in the left parietal region. The hair in it was characteristically broken off. However, the parents associated the appearance of this lesion not with contact with the kitten, but with a fall from a bicycle, a superficial abrasion and its contamination, especially since both events coincided in time. The lesion was therefore considered pyodermic. Treatment with corticosteroid creams and antibacterial agents provoked the spread of the fungal process to the entire left half of the head. Due to swelling, infiltration, suppuration, enlargement of the cervical and preauricular lymph nodes, the head and face seemed asymmetrical. The surface of the skin in the focus of mycosis was covered with rough purulent and purulent-bloody crusts with sparse hair stuck together in them. At the slightest movement of the head and neck, the child experienced severe pain. The boy was lethargic, apathetic, pale, and there were periodic rises in temperature. Along with the atypical focus of mycosis described above, characteristic small foci of mycosis appeared on the head in the area of the left eyebrow, on the forehead and temple. Fluorescent examination revealed a typical green glow in them. The diagnosis was confirmed microscopically and by isolating an identical culture of fluffy microsporum from all foci of mycosis.
Infiltrative-suppurative microsporia of the skin of the pubis and labia can be classified as atypical in localization and course. This form of microsporia often (according to our data, in two out of five cases) leads to infection of sexual partners. Due to the atypical localization and course, this form of microsporia is not immediately diagnosed. Erroneous and inadequate treatment makes clinical manifestations even more uncharacteristic.
Currently, the localization of microsporia foci on the skin of the pubis and labia has increased more than tenfold compared to 1976. The peculiarities of the anatomical structure of this area, replete with blood vessels and nerve endings, contribute to the rapid formation of deep invasive, extremely painful infiltrates, the appearance of complications in the form of lymphadenitis and allergic rashes, and the appearance of symptoms of intoxication due to the absorption of lysed tissues, bacteria, fungi and their metabolic products.
We present in more detail the medical histories of two women, one of whom infected her sexual partner, the other herself was infected during sexual contact.
An 18-year-old woman had no diagnosis of microsporia for four months. She became infected from her nephew, who had microsporia, by using a washcloth to wash him. A superficial focus of microsporia on the skin of the inguinal fold resolved after a week of lubrication with a 2% iodine solution. The patient considered the episode to be over. Therefore, when, after a month and a half, superficial flaky lesions appeared on the skin of the pubis, she in no way connected them with untreated microsporia. Application of corticosteroid creams (suspicion of allergic rashes), frequent sea bathing (the patient was at sea at that time) and almost constant stay in a tight-fitting bikini led to the spread of the pathological process both on the surface and in depth. Folliculitis, perifolliculitis, and abscess elements formed, merging into a single conglomerate rising above the surface of the skin. “Dropouts” appeared on the anterior surface of both thighs and the skin of the lower abdomen (Fig. 4). The surface of the foci of mycosis was covered with rough purulent and purulent-bloody crusts. The inguinal lymph nodes became enlarged and painful. Painful subcutaneous nodes appeared on symmetrical areas of both legs. The disease was regarded as deep ulcerative-vegetative pyoderma, complicated by erythema nodosum of the legs. The patient was unsuccessfully treated with oxacillin, kefzol, vibramycin in combination with short courses of prednisolone. The pain and symptoms of intoxication only increased. The diagnosis of microsporia was helped by the appearance of a typical focus of mycosis on the skin of the abdomen of the patient’s sexual partner. After a detailed examination of the woman, as the presumed source of microsporia, her infiltrative-suppurative form was diagnosed. The clinical diagnosis was confirmed microscopically, fluorescently and culturally.
A 25-year-old patient who became infected with microsporia from a patient had a similar history of the disease. A week after sexual contact, a bright itchy spot appeared above the pubis, quickly becoming covered with scaly crusts. The patient was being treated for ureoplasmosis at that time, and the spot was regarded as allergic. Under the influence of short therapy with Triderm cream, the spot faded and became almost invisible. A month after this episode, while staying at sea, superficial scaly rashes appeared on the pubic skin, merging into a large area of curly outlines. Deciding that these were allergic rashes, the patient used Lorinden cream and 2% salicylic alcohol. For ease of lubrication, the patient shaved her pubic hair. This provoked the process to spread into depth. An extremely painful infiltrate of deep follicular nodular elements formed. Deep pyoderma was diagnosed. Tsifran and vilprofen were used orally, fucarcin and lincomycin paste were used externally. However, pain, infiltration and impetiginization only increased. To clarify the diagnosis, after two months from the onset of the disease, the patient was sent to the Central Clinical Hospital.
On the pubis, occupying its entire central part, passing onto the skin of the outer labia and twisting into cords in the upper and lateral parts, there was an extensive infiltrate, rising 1-2 cm above the skin level. Its contours were emphasized by a bright peripheral ridge. The skin over the focus of mycosis was bluish-brown, tense, stretched, with a bumpy surface (Fig. 5). Touching the hearth turned out to be unusually painful. The pubic hair completely retained its length; the cap usual for microsporia was not visible. The central part of the lesion was practically devoid of hair. The remaining hair was difficult to epilate, and epilation was accompanied by severe pain. The inguinal lymph nodes were enlarged and painful. Papulovesicular microsporidae were present on the dorsum of both hands. A luminescent examination of the focus of mycosis on the pubis and labia revealed a characteristic green glow. Microscopic examination revealed small spores located on and inside the hair. A typical culture of fluffy microsporum was obtained on a nutrient medium.
Treatment of patients with microsporia seems to be an important, socially significant problem.
This disease usually affects not only children, but also their parents. Due to the high contagiousness of mycosis, children are prohibited from attending kindergartens and schools. They miss school classes and find themselves separated from the children's group for a long time. Parents are forced to interrupt work and take sick leave for care. Thus, the family suffers significant moral and material damage.
A speedy recovery of patients with microsporia is achieved with timely recognition of mycosis and adequate treatment. It includes the combined use of systemic and external antifungal agents along with pathogenetic drugs. The latter increase the effectiveness of treatment and reduce the frequency and severity of adverse reactions and complications.
In patients with microsporia, two systemic antimycotics are used: the antibiotic griseofulvin and lamisil. Moreover, antimycotics are used in high doses in patients with microsporia. The fact is that the causative agent of mycosporia is characterized by the highest resistance compared to other dermatophyte fungi. For example, the daily dose of griseofulvin, equal to 16 mg/kg in patients with rubrophytosis and 18 mg/kg in trichophytosis, should be increased to 22 mg/kg for mycosporia. The high stability of fluffy microsporum spores is due to the presence of a very dense six-layer shell, reinforced by longitudinal and circular costal projections [11].
Griseofulvin is a chlorine-containing antibiotic, a product of biosynthesis of mold fungi of the genus Penicillium. Therefore, when taking griseofulvin and simultaneous treatment with penicillin antibiotics, mucocutaneous allergic complications very often occur. The daily dose of griseofulvin, which is selected at the rate of 22 mg per kilogram of weight, is divided into three to four equal parts and taken with one teaspoon of vegetable oil. The oil stimulates the evacuation of bile and promotes the dissolution of griseofulvin. In addition, due to the presence of vitamin E (a-tocopherol), the metabolism of griseofulvin slows down and the duration of action of the drug increases. Griseofulvin is better absorbed in an acidic environment, so it is advisable to drink it with some sour juice (lingonberry, cranberry, lemon, apple, etc.).
To reduce the hepatotoxicity of griseofulvin, it is recommended to take it with hepatoprotectors - liver preparations, Liv-52, Karsil, Silibor, etc.
Given the poorer absorption of griseofulvin in the presence of helminths, deworming is indicated before or during griseofulvin therapy [8]. For this, various anthelmintic drugs are prescribed, for example, decaris (levamisole), which eliminates helminths and at the same time has immunomodulatory properties. Griseofulvin somewhat enhances immunodeficiency conditions, against which, as a rule, microsporia occurs. Levamisole neutralizes the immunosuppressive effect of griseofulvin. During griseofulvinotherapy, foci of focal infection usually worsen, which become sources of superinfection of foci of mycosis, therefore their sanitation is indicated.
The course of continuous treatment with griseofulvin lasts 1.5-2 months. Initially, it is used daily until two negative fungal tests are obtained seven days apart; then the antibiotic is used for two weeks every other day and another two weeks twice a week. At the end of therapy, a control clinical and laboratory examination is carried out, and in case of negative results, the patient is considered cured. Although griseofulvin is a fairly gentle drug, it still has hepato-, nephro- and neurotoxicity, photosensitizing, embryotoxic and cocarcinogenic properties.
Griseofulvin is contraindicated in hepatitis that was suffered no more than a year ago and is manifested by subjective sensations and/or elevated levels of bilirubin and liver enzymes; peptic ulcer of the stomach and duodenum; kidney diseases; neuritis, especially of the optic and auditory nerves; malignant and fast-growing benign tumors; blood diseases; photodermatoses and related conditions; cerebrovascular accident; uterine and other bleeding.
It should be taken into account that an adequate dose of griseofulvin in patients with microsporia should not exceed the maximum permissible - 1.0 g (8 tablets). Otherwise, the toxic-allergic properties of the antibiotic appear. In adults and large children weighing more than 60 kg, prescribing an adequate dose of the drug is practically impossible.
A worthy alternative to griseofulvin is terbinafine (trade name Lamisil).
The drug has high activity against various types of fungi. It is especially active against dermatophyte fungi, the causative agents of the most common dermatophytosis: rubrophytosis in adults and microsporia in children.
Lamisil suppresses squalene epoxidase, which is extremely sensitive in fungi (10 thousand times more sensitive than in humans). As a result, at the very early stages (at the level of the squalene epoxidase cycle), the formation of ergosterol, the main component of the cytoplasmic membranes of the fungal cell, is blocked. Without receiving this building material, the fungal cell becomes defective, cannot grow and develop, but only survives. This is how the fungistatic effect of Lamisil manifests itself. However, the predominant fungicidal effect of this antimycotic is. It directly depends on the accumulation of squalene in the cell, excluded from the cycle of further transformations into ergosterol. These active high molecular weight hydrocarbons accumulate in the fungal cell. Moreover, the volume of squalene granules gradually increases, since they actively extract lipids from cell membranes. Ultimately, a cell membrane with a damaged structure cannot withstand it and ruptures, leading to cell death [6, 7].
Lamisil does not require any specific conditions for administration and is quickly absorbed from the gastrointestinal tract. Its blood level is stable. The drug practically does not interact with various medications, as well as enzyme systems, including cytochrome P-450. Its action is selective and directed mainly at the fungal cell. Lamisil enters the skin and its appendages by simple diffusion, as well as excretion by the sebaceous glands.
The peculiarities of the distribution of Lamisil due to its lipophilicity and connection with chylomicrons include its lymphatic transport. Through the lymphatic vessels, Lamisil directly reaches infiltrative-suppurative and abscessing foci of mycosis with lymphadenitis and lymphangitis. In this regard, the greatest activity of Lamisil is observed in patients with severe complicated infiltrative-suppurative forms of dermatophytosis with hair damage. According to M. Tsoi and M. D. Alaeva (1996), with superficial trichophytosis, lamisil accelerated the recovery process by 3.3 days, with infiltrative trichophytosis - by 6.3 days, with suppurative trichophytosis - by 8.2 days compared with griseofulvin therapy [10].
The rapid resolution of complicated forms of dermatophytosis during therapy with Lamisil is thus associated with its high antifungal activity, lymphatic transport, pronounced antibacterial properties comparable to the action of gentamicin, as well as anti-inflammatory effect. The latter is due to the suppression of peroxidase activity of hydroxyl radicals of polyunsaturated fatty acids.
Above, we have already noted the high resistance of fluffy microsporum to antimycotics. In this regard, N. S. Potekaev et al. (1997) observed the cure of children with microsporia with lesions of long and vellus hair, who were prescribed Lamisil 94 mg per day with a body weight of up to 20 kg and 186 mg per day with a body weight of 20 to 40 kg, which is 50% higher than the dose, proposed in the annotation for the drug [4].
In adults with complicated forms of microsporia, we successfully carried out short but intense courses of therapy with Lamisil. The drug was prescribed at a daily dose of 7 mg/kg or two tablets (500 mg) per day. In the next three to four weeks, we observed complete resolution of microsporia foci in all patients without exception. Healthy hair began to grow where scar atrophy had not developed, microsporidae, including foci of erythema nodosum of the legs, simultaneously resolved, regional lymph nodes became painless and decreased in size. In no case were any side effects or deviations in the biochemical status noted [6].
I would also like to note the better tolerability of Lamisil compared to its analogue, Exifin. One of our patients began, on her own initiative, to take the cheaper exifin instead of Lamisil. After four to five days of taking exifin at a daily dose of 500 mg, itchy papulovesicular allergens appeared on the inner surface of both forearms. They resolved after the use of adsorbents and antihistamines. After resuming therapy with lamisil at a daily dose of 500 mg, allergens did not appear.
And one more thing: in the family of one of our patients, everyone except her had respiratory infections. We associated its stability with an increase in the body's defenses as a result of taking Lamisil. It is known that Lamisil does not have a negative effect on the metabolic activity of leukocytes, chemotaxis, and phagocytosis. Moreover, under the influence of lamisil therapy, indicators of cell-mediated immunity improve, which is associated with the release of large amounts of antigenic material as a result of the death of fungal cells [12].
The effectiveness of treatment of patients with microsporia increases with the simultaneous use of systemic antimycotics and external agents. Along with epilation and weekly shaving of hair, a 2% tincture of iodine is used, which is used to lubricate the foci of mycosis in the morning. In the evenings, domestic antifungal ointments are rubbed into them: sulfur-salicylic, sulfuric, sulfur-tar, bifosin. This iodine-ointment treatment is highly effective and cheap and accessible.
For relatively calm foci of microsporia, it is advisable to lubricate them once a day with 10% salicylic-quinosol dimexide, which quickly leads to the resolution of foci of mycosis on the scalp.
For infiltrative-suppurative microsporia, to free foci of mycosis from crusts and pus, compress bandages with 10-20% solutions of ichthyol, 5% solution of mumiyo in dimexide, 50% solution of licorice root, as well as lotions with 0.5 -1% solutions of chlorhexidine bigluconate (Ghibitan) or ultrasonic irrigation with a 0.5% solution of this drug using the Rossa apparatus [2, 5].
Effective foreign azole and allylamine compounds can be used as external antimycotics. Among them, we prefer Lamisil 1% cream, Mycosporus 1% cream and Travogen 1% cream. These drugs are usually well tolerated because they have anti-inflammatory properties. In case of acute inflammatory phenomena, their combination with corticosteroids is not required. At the same time, they have pronounced antifungal activity, and lamisil cream also has an antibacterial effect, which is important for the rehabilitation of microsporia foci complicated by secondary pyococcal flora.
The inclusion of external antifungal agents in the complex of treatment measures for patients with microsporia allows one to achieve rapid recovery with the smallest course dose of expensive systemic antimycotics that are not indifferent to the body.
Tests and diagnostic methods
All tests and diagnostic methods are extremely important, as they quickly determine whether a cat has a fungal infection, which is also dangerous for humans. Today, veterinarians around the world use three main methods:
- Wood's lamp. This is a special lamp that uses a UV radiation source as a lamp. A sort of mini-solarium. The essence of his work is that under ultraviolet light, some strains of dermatophytes begin to fluoresce. Accordingly, in cases where a cat’s fur begins to glow, like a neon sign in a store, a positive diagnosis of microsporia can be confidently made.
- Microscopic examination of hair samples and skin scrapings from the boundaries of healthy and diseased tissue. The most common and “simple” method. The complexity of the study prevents us from calling it simple without quotation marks: only an experienced veterinarian will be able to detect the mycelium of parasitic fungi.
- Growing a pathogen culture on a nutrient medium. The most reliable, but complex and time-consuming method. Fungi need a specific and expensive environment, and they grow on it for a long time. Therefore, the technique, even if it produces a 100% result, is used, rather, not to make, but to confirm the diagnosis after the fact.
Diagnostic measures
Diagnosis and treatment of ringworm are carried out by a dermatologist. The doctor examines the patient and identifies typical manifestations of microsporia. Examination of skin scrapings under a microscope reveals fungal mycelium and changes in the structure of hair and skin. Differential diagnosis makes it possible to exclude trichophytosis from the patient’s history, which has similar manifestations upon microscopy of the patient’s biomaterials.
Microflora culture appears to be a more informative diagnostic technique. Laboratory staff determine the type and genus of fungi. Based on the laboratory report, the dermatologist selects drugs that will cure the patient.
Luminescent examination makes it possible to identify pathological lesions on the skin of the patient and those living with him. This diagnostic method is based on the green glow of the fungal mycelium under the influence of a gas-discharge light source.
Treatment of microsporia in cats
I would like to immediately note that the treatment of microsporia in cats is a rather lengthy process that requires patience and time. You should not count on a quick recovery for your pets.
Important! If the cat is not treated, the animal will either become a carrier, or the disease will become latent, chronic. It is even more difficult to cure, and all this time the pet will continue to remain infectious to other pets, as well as owners.
It is possible to stop treatment, considering the cat to have recovered, only after a thorough veterinary examination and at least two negative microscopic examinations of the skin and fur.
And further. The medications used in the treatment of severe and advanced forms of the disease are very “severe”; their long-term use is fraught with the development of problems with the kidneys and liver. Therefore, it is better not to let things get to this point, starting treatment for microsporia immediately after diagnosing the disease.
Approximate treatment plan
The treatment regimen below is just an approximate one, it needs to be modified for each specific case, taking into account the characteristics of a particular animal (consultation with a veterinarian is also required):
- First, the pet is prepared for treatment. To do this, you need to carefully trim the hair around the lesions. If the cat has long hair, it is generally advisable to trim it entirely. This measure will greatly facilitate mandatory medical procedures, including the application of ointments and other antifungal drugs.
- Apply antifungal ointments to both the affected areas and the skin around them. It is necessary to capture at least a centimeter of healthy tissue. This will prevent further spread of the pathogenic fungus. Ointments must be applied daily.
- Sick cats must be washed with shampoos with antifungal and keratolytic effects. This allows you not only to destroy the pathogen, but also to cleanse your pet’s skin of crusts, scabs and scabs. This is not done for the sake of improving the appearance of the pet (although for this purpose too): it is easier to apply medications to clean skin and they act much faster. As a rule, in the initial stages of treatment, washing should be done every three days, and subsequently the frequency of treatments can be reduced to twice a week.
- Antifungal agents are prescribed in the form of injections or tablets for oral use. The frequency of their use is determined by the veterinarian. You should not do this yourself, as you can easily poison your pet.
- If the case is severe and the pet will have to be treated for a long time, he must be prescribed multivitamins and immunostimulants. This will keep the cat healthy and speed up the normalization of its condition.
Medications
We list the main drugs used by veterinarians in the treatment of not only microsporia, but also trichophytosis and other dermatophytes:
- Ointment Yam. The drug is “simple”, it has a not very pleasant smell and an extremely sticky consistency, which is why letting a cat smeared with it on the sofa or bed is not the best idea. But the medicine is cheap and quite effective. For microsporia, use it at least three times a day, generously lubricating the lesions on the skin.
- Ivamerol. A product that has gained special recognition in recent years from many veterinarians and cat lovers. Before use, the drug solution is diluted in water (preferably boiled and settled) in a ratio of 20 ml of the composition per liter of water. The amount of mixture is calculated in such a way that it hides the cat seated in it up to the neck. Exposure duration is at least five minutes.
- Intraconazole-based products. Prescribed in a dose of 10 to 18 mg per kilogram of the cat’s live weight (at the discretion of the veterinarian). Since these medications negatively affect the liver of animals, hepatoprojectors (Essentiale-Forte and the like) are additionally prescribed.
Folk remedies
In general, we would not recommend using folk remedies for microsporia, especially in severe cases. They are not particularly effective, but they can easily trigger and complicate the disease. But still, for superficial microsporia, the following is sometimes used:
- A mixture of tar and laundry soap in a 1:1 ratio. First, the “raw materials” are grated on a fine grater and slightly heated in a water bath to obtain a semi-liquid slurry. It is applied to the lesions (but the composition should not be hot) three times a day. Exposure time - 15 or 20 minutes. If signs of irritation appear, the exposure period is reduced to 6-7 minutes.
- Birch tar, but in the case of cats its use is contraindicated. If there are no alternatives at all, a small amount of tar is applied to the affected areas of the skin for 15 minutes, and at this time a surgical collar is put on the animal or held so that the cat does not lick the smeared areas. Then the tar is thoroughly washed off with warm water and baby soap. If your pet gets tarred, it may die.
- Alcohol tincture of iodine. They lubricate the lesions twice a day.
Reviews
Ringworm in its advanced form is very difficult to treat, but this is not a death sentence and we must definitely fight. The Polivac vaccine did not help my cat, the Itracon capsules did not help, he only developed severe hepatitis and he almost died. Due to the treatment of hepatitis, they temporarily stopped treating lichen, the liver failed and the cat was actually dying, there was no time for lichen. For 3 months, about 25–30% of the cat’s skin was damaged and scratched, everything was covered in bloody wounds and scabs, it was constantly itching. I put on a sweater so that I would comb my hair less. After hepatitis, there was no talk of any medications or ointments; only Imaverol was allowed. After 2 days for 3, I smeared it not on the whole cat, but only on the lesions and around them, and on the doctor’s advice I diluted it not 1:20, as written in the instructions, but first for about a month I diluted it 1:5, then 1:10 . At the beginning of treatment, she was given the immunostimulant Cycloferon in parallel. I was treated for 2.5 months, the first month it generally seemed to me that the lesions were only growing and nothing was helping. After about a month, new lesions stopped appearing and gradually began to heal, the scabs fell off and became overgrown with hair. The fur, of course, was in terrible condition after that, I was pierced with vitamins Gepavi-kel and Tetravit and the cat was transformed before our eyes, now he is a fluffy handsome man. I vacuumed and washed the premises, but didn’t really treat them; it’s simply impossible to treat them properly at home. Don't give up and don't despair, everything will work out for you.
Svetlana
https://forum.ua-vet.com/viewtopic.php?f=23&t=52776
When we were covered with a fungus, Griseofulvin helped us. It may seem too harsh to some, but we didn’t come to him right away either, it’s a pity they didn’t tell us about him earlier, and so we had to feed the entire herd with Griseofulvin. But the results were noticeable after about the first week. Give 1/6 tablet once a day. Those who have not become infected can take it for a week; patients who are sick need a course of 3-4 weeks, even if everything goes away in 1-2. But Fungin is still not worth it for a small kitten, he is very vigorous, the kitten can puke on him and, excuse me, he can vomit... Isolate the small one if possible. Well, wash the apartment with some special means, or just vinegar water.
sanguiss
Caring for a sick cat
Caring for a sick cat is no different, but... With microsporia, the main rule of care is to make sure that other pets and people themselves do not suffer. Therefore, the following rules must be observed:
- If the cat has long hair, then, as we have already said, it needs to be cut. All wool must be collected and burned to prevent the spread of infection.
- A sick pet needs to eat well and properly (to prevent “sagging” immunity), and therefore it is either transferred to high-quality “natural” food or holistic food.
- To prevent the spread of infection throughout the apartment, we highly recommend limiting the movements of a sick cat to one room. And, by the way, it is necessary to carry out wet cleaning every day, and ideally even carry out quartz treatment.
Factors of occurrence
The occurrence and development of the pathological process can be influenced by several reasons:
- reduced activity of the pet's immune system;
- influence of stressful situations;
- inappropriate hygiene requirements in the premises;
- injury to the skin.
The disease can occur in cats at any age. The risk group includes newly born kittens and animals living on the street.
Vaccination and vaccines as a way to prevent and treat microsporia
Since the disease we are describing is quite dangerous (including for humans), scientists have long been researching the possibilities of preventing it. This is how vaccination and vaccines against microsporia appeared. They are unique in that you can vaccinate not only healthy cats, but also already sick cats (i.e., these vaccines can act as medicine).
Domestic experts recommend using the following varieties:
- Polivak-TM. Dose – 0.6 ml per administration. For prevention, vaccination is necessary; during treatment, it is repeated after two weeks.
- Vakderm. Dose: 0.5 ml per cat. Unlike the previous drug, revaccination is mandatory after two weeks (regardless of the purpose of using the vaccine).
Both products do not provide 100% protection for your pet from microsporia, but they significantly reduce the risk of developing severe forms of it and significantly speed up recovery.
Prevention of microsporia
All prevention of microsporia is as follows:
- If the area is unfavorable due to illness, you should not let the cat go outside again, thereby protecting it from contact with stray animals.
- For walks on the street, it is better to use a harness that will prevent the animal from running.
- Your pet should be vaccinated against microsporia at least once a quarter.
- Do not develop other diseases that lead to a severe weakening of the immune system.
Causes and provoking factors
The disease is caused by the causative agent of lichen, which is transmitted from a sick animal to a healthy one through direct contact, as well as through common objects: blankets, toys, dishes. Only an animal with a weakened immune system can become infected; this condition is predisposed to:
- persistent infections;
- parasites;
- constant stress;
- poor nutrition;
- vitamin deficiencies;
- long-term use of medications.
In such conditions, the body's resistance to microbial agents that can cause infection decreases. The fungus quickly affects the layers of skin, hair and nails.
Disinfection of living quarters
In order not to become infected yourself and not to endanger your family, you must always remember: high-quality disinfection of a living space is the key to health.
You need to do the following:
- The room with a sick cat is wet cleaned daily. At the same time, “killer” amounts of chlorine bleach are added to the water. Since cats do not like chlorine, after this everything is washed off with clean water and the room is ventilated.
- The floors in the house are vacuumed regularly. After this, it is advisable to burn the dust collection bags, and wash the containers of vacuum cleaners with water cleaning with the same chlorine-containing products.