Feline hemobartenellosis (or infectious anemia) is a blood-parasitic disease, similar in its clinical manifestations to piroplasmosis (babesiosis) in dogs. This is a contagious disease, the typical clinical sign of which is anemia as a result of massive death (hemolysis) of red blood cells (erythrocytes). The occurrence of the disease is possible at any age in individuals of any sex, but males suffer from hemobartonellosis more often than cats (this is most likely due to more aggressive behavior and constant struggle for territory, fights, and, as a result, a greater likelihood of infection). Carriage is widespread in the cat population, especially stray cats, but the clear clinical picture usually manifests itself in cats in an immunosuppressed state, in the presence of concomitant inflammatory or infectious diseases, for example, the cause can be any lethal chronic viral infection: feline leukemia virus (FeLV) , feline immunodeficiency virus (FIV) or feline infectious peritonitis virus (FIP).
What is infectious anemia in cats?
Feline infectious anemia (FIA) is a parasitic blood disease caused by the grain-like bacterium Haemobartonella felis. After entering the body, the pathogen damages the outer membrane of red blood cells, reducing the life of red blood cells by 2 times.
To destroy invaders, the immune system produces special antibodies that attack infected cells. Some healthy red blood cells come under attack - this is due to the production of autoimmune antibodies that mistake their own cells for enemies.
Due to the premature destruction of red blood cells, the infected animal develops anemia. Lack of oxygen leads to weakening of the functions of internal organs and tissue death.
Pathogenesis of hemobartonellosis
The carrier becomes infected with Bartonella when bitten by an infected animal. In the intestines of fleas (ticks), they multiply and are excreted with feces into the environment (including onto the cat’s fur). In case of injuries or scratches, Bartonella enters the skin, where they are presumably ingested by tissue macrophages (monocytes), multiply in them and migrate into the bloodstream. Some Bartonella penetrate into the endothelial cells of the inner surface of blood vessels, some into erythrocytes, where further reproduction occurs. The cycle repeats when the infected cat is bitten again by the carrier.
Bartonellas have a number of features and adaptations
, which avoid a pronounced immune response in the animal.
Firstly
, they are localized inside red blood cells without causing hemolysis, which prevents their antigens from being detected by lymphocytes.
Secondly
, they are able to change and hide the pathogen-associated protein pattern on the surface of their membrane, which complicates their recognition by dendritic cells.
The latter are involved in the recognition of foreign antigens. Thirdly
, Bartonella secretes interleukin-10, which inhibits the production of T-lymphocytes (helpers), monocytes, and dendritic cells. As a result, a decrease in the production of protective immune cells leads to prolonged and severe bacteremia (2 years or more).
Causes and routes of infection
The disease is transmitted through the blood of cats infected with hemobartonellosis. This happens when:
- receiving wounds in fights;
- blood transfusion (transfusion);
- bites of ticks and fleas - the main carriers of hemobartonella.
Another possible route of transmission is transplacental. The asymptomatic form of the disease during pregnancy sharply turns into the active phase. The mother's bacteria are passed through the placenta to the kittens, causing their death.
The risk group includes males under 3 years of age who are suffering from acute pathology. In cats, chronic hemobartonellosis is more common, worsening for the following reasons:
- presence of tumors;
- prolonged stress;
- lack of vitamins or low calorie diet;
- recent surgery;
- addition of a secondary infection.
Animals that have suffered an acute form of the disease continue to be carriers even after recovery. Despite this, the possibility of transmission of infection at this stage has not been proven.
Symptoms of infection
The first symptoms appear on days 8-17 of infection. Increasing weakness associated with a drop in hemoglobin levels is accompanied by apathy, fatigue, increased sleep duration and decreased appetite. In addition to behavioral changes, others are added over time, including:
- paleness of the tongue and gums;
- shortness of breath (the cat breathes only with its mouth open);
- increase in heart rate above 180 beats per minute;
- yellowing of the mucous membranes and skin, as well as darkening of the urine associated with the accumulation of hemoglobin in the liver;
- enlarged lymph nodes;
- dry skin and deterioration in coat quality (alopecia areata and unkempt appearance).
Fever is rare and is not a specific sign of IAC. Its appearance is caused by an acute form of the disease, the addition of a secondary infection or an inflammatory process (inflammation of the testicles in males). In all of these cases, the body experiences severe intoxication, requiring immediate veterinary care.
The severity of symptoms depends on the strength of the immune system and the course of the disease. The least pronounced symptoms are characteristic of the chronic form, and the most pronounced - for the acute form. In the latter case, the rapid destruction of red blood cells leads to severe cardiovascular failure followed by loss of consciousness.
Death can occur within a few hours after the first alarming signs and symptoms appear, so it is better not to delay treatment of hemobartonellosis in cats.
Diagnosis by laboratory tests
The main research method is a blood test. With its help, veterinarians determine the presence of a pathogen and exclude pathologies with similar symptoms: immunodeficiency virus and viral leukemia.
Basic methods for diagnosing hemobartonellosis in cats include:
- General and biochemical blood test
. The results of the study confirm severe anemia, accompanied by a decrease in hemoglobin and hematocrit against the background of an increase in reticulocytes (immature red blood cells). There is also an increase in the bile pigment - bilirubin, which is formed during the breakdown of red blood cells.
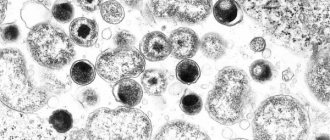
- Light microscopy
. When affected by hemobartonella, a change in the contour and color of red blood cells is observed in a stained blood smear. Their edges become uneven and convex, and single or multiple (2-6 pieces) inclusions of bacteria appear on the surface. The disadvantage of this method is its inaccuracy due to the rapid settling of the solution and the transience of the life of the parasites. At the time of analysis, they may simply not be noticed.
- Abdominal ultrasound
. Due to anemia, the spleen enlarges. The change in size is due to the abundance of damaged red blood cells, which she needs to remove from the body. As the organ grows, it captures more and more cells, aggravating the existing anemia.
- Polymerase chain reaction (PCR)
. Allows you to detect DNA fragments of the pathogen before the first symptoms appear.
Six months after the end of treatment, PCR is repeated. If the result is negative, then the animal is considered healthy.
Symptoms of the disease
Once in the cat's body, Haemobartonella felis attaches to the membranes of red blood cells and destroys them, as a result of which the life span of the cells is significantly reduced and the cat develops anemia. The structural components of the liver, spleen, bone marrow and lymph nodes suffer most in this case.
Sick cats may experience:
- increased heart rate and breathing;
- dryness and flaking of the skin, loss of elasticity;
- ruffled and dull fur, baldness;
- blanching and yellowing of the mucous membranes;
- dark coloration of urine;
- decreased physical activity;
- refusal of food;
- distortion of taste perceptions - the pet can eat sand, chalk, dirt, etc.
- swollen lymph nodes;
- hoarseness of voice;
- weight loss
For your information. Clinical signs of the disease are observed in only 30% of affected cats. Other animals become carriers of the disease.
The following is detected in the blood of sick animals:
- changes in the size and shape of red blood cells;
- an increase in the number of immature blood cells;
- increase in bilirubin levels;
- red blood cells stained with both basic and acidic dyes (polychromasia).
Be sure to read:
Sepsis in cats, causes, symptoms and treatment, recommendations from veterinarians
The diagnosis is made by a veterinarian based on examination and test results of the animal.
Treatment and likelihood of recovery
Recommended therapy is divided into specific and symptomatic. The first is aimed at destroying hemobartonella in infected cats, and the second is aimed at eliminating the symptoms of the disease.
To combat parasites, tetracycline antibiotics (Doxycycline, Oxytetracycline) or fluoroquinolones (Enrofloxacin, Baytril) are used. The duration of antibiotic therapy ranges from 10 to 28 days.
The symptomatic treatment regimen includes:
- blood transfusion, vital when the hematocrit drops below 15%;
- hormone therapy (glucocorticosteroids), which suppresses the work of autoimmune bodies;
- taking multivitamin preparations that stimulate the regeneration of dead red blood cells;
- infusion therapy (droppers), restoring the water-salt balance;
- a high-protein diet that improves the transport of iron within the body.
Despite anemia, iron-containing drugs that increase the level of hemoglobin in the blood are not used. Due to accelerated hemolysis (destruction of red blood cells), this indicator, on the contrary, has to be artificially reduced.
Features of kitten treatment
Due to their weak hematopoietic and immune systems, kittens are very susceptible to the disease and often die from cardiac arrest caused by severe exhaustion. Antibiotic therapy is not suitable for children - the drugs used have a negative effect on the formation of the skeletal system, and their toxicity causes vomiting and tissue death at the injection site.
The only possible treatment is the use of antiprotozoal drugs. They help only with the slow development of the disease. In other cases, the prognosis for the pet is unfavorable. With a stable deterioration of the condition, veterinarians recommend euthanasia.
Care and nutrition
Like all sick people, your pet will need complete rest and a comfortable place. Place the bed in a warm place away from the noise of the TV and ask children to temporarily stop playing with the cat.
The tray can be left in its usual place, but for safety you should buy diapers - if the cat is very weak, he can urinate right on the bed, so he will have to be washed and transferred to a clean bed. You will also have to pay attention to the wool. Brush it regularly to maintain a neat appearance.
To regulate hemoglobin levels, you need to add foods rich in heme iron to your diet. It is well absorbed and is found in foods of animal origin:
- pork heart and lungs;
- beef liver and meat;
- blood of cattle.
Food can be given boiled or raw. In the latter case, choose trusted suppliers to prevent infection by parasites. If the pet refuses to feed, then food must be administered intravenously in a hospital setting.
Forecasts
An unfavorable prognosis is given not only at a young age, but also in the presence of concomitant infections. The situation is especially dangerous when an animal is diagnosed with viral leukemia. In this case, the bone marrow loses the ability to regenerate red blood cells, and recovery becomes impossible. Any improvements have a short-term effect, so pets with such a disappointing diagnosis are euthanized.
Another sad scenario is a latent form of infection. Due to the prolonged absence of symptoms, the body suffers from oxygen starvation for a long time. At the time the disease is detected, the animal is too weak to tolerate toxic drugs. He can only be saved by a blood transfusion, but this method of treatment is only available in large cities.
Upon recovery and negative results of repeated PCR, the pet continues to remain a carrier. Any decrease in immunity can lead to relapse of the disease.
Pet care
The first step if your pet has contracted hemobartonellosis is to ensure complete rest. To do this, the bed is moved to a quiet, warm place. The litter tray should not be moved. It is advisable to prepare a spare sleeping place, since the pet can “walk under itself” due to weakness. If the cat completely refuses to eat, you have to force-feed it (the best option is intravenous administration of protein hydrolyzate in a hospital).
Due to weakness, the animal cannot lick itself, so the owner will have to take care of the fur. The cat is regularly and carefully combed, and if necessary, the fur is moisturized. To avoid difficulties with giving capsules or tablets, it is recommended to use a piller. The tablets are given with water or broth to make swallowing easier.
Vaccination and prevention
There is no vaccine against this disease, so the only way to prevent it is regular treatment against blood-sucking parasites. Acaricidal and repellent preparations are produced in the form of drops, sprays and collars. Each of them has its pros and cons, which you should familiarize yourself with before purchasing.
Also try to avoid contact with stray animals. They are often infected with parasites and can infect your pet even after short-term contact. Parasites can be brought into the house on your own shoes or clothes, so the quality of disinfection of basements in apartment buildings plays a big role. On this issue, you can contact the management company or seek private services.
Feline infectious anemia is a dangerous parasitic disease that is often fatal. To protect your pet, it is important not to forget about preventative treatment and seek help with any changes in habitual behavior. The earlier the infection is diagnosed, the greater the chance of a favorable outcome without complications.
The article is for informational purposes only. Contact your veterinarian!
Do you like the article? 186
Danger to people
Hemobartonellosis is an infectious disease, so it is quite natural to find out whether it is contagious to people or other pets? Veterinarians are convinced that Bartonella does not belong to zooanthroponoses, which means that they do not threaten humans in any way.
In addition, they are harmless to dogs. They have their own disease with a similar name, but it is provoked by a different type of infectious agent. So hemobartonellosis poses a danger exclusively to representatives of the cat family.