Diabetes mellitus in cats is one of the most common diseases of the hormonal system, which is based on a violation of carbohydrate metabolism. The pathology mainly occurs in older animals, more often in neutered cats than in cats. In this article we will talk about why diabetes occurs in cats, why it is dangerous, and how to treat it.
Definition of disease
Diabetes mellitus belongs to the group of endocrine diseases. One of the characteristic symptoms of this disease is unquenchable thirst and frequent urination, resulting in dehydration. There is an increased sugar content in the blood and urine.
This condition threatens the animal's life. In diabetes, the pancreas produces little or no insulin. Glucose and sugar entering the body are not broken down; they enter the blood unchanged and then enter the urine. As a result, metabolic processes throughout the body are disrupted.
Insulin is a protein. Its main function is the breakdown of glucose. It is not produced by the entire pancreas, but by its beta cells. They are located among the gland tissues on the so-called islets of Langerhans.
Beta cells die for various reasons. When their number decreases catastrophically, insulin will cease to be produced. The development of diabetes mellitus is an inevitable consequence of these disorders.
Why are glucose and insulin needed?
Glucose is absorbed into the blood from the intestines and then enters cells throughout the body. Insulin is needed for glucose to enter cells.
Glucose is a type of sugar. It is formed when the body breaks down nutrients. Glucose is a source of energy for organs and cells of the body.
Insulin is produced by the pancreas. This hormone is responsible for ensuring that glucose enters cells and organs. Insulin is like a key that opens a channel in cells for glucose to enter.
Insulin tells cells to take up glucose
Types of diabetes in cats
There are 3 types of diabetes in cats. In humans, the disease is chronic and incurable; only correction of the condition and supportive therapy are possible. In cats, the situation is not so sad - the second and third types are curable with adequate treatment or elimination of the cause of the disease.
First
This type of diabetes mellitus is rarely diagnosed in cats. The animal's pancreas does not produce insulin on its own due to the death of all beta cells, so its absolute deficiency develops. If the cat is not provided with insulin replacement therapy, the development of ketoacidosis is inevitable. The next stage is coma.
Second
In cats with type 2 diabetes mellitus, insulin is produced in sufficient quantities. However, tissues and organs do not respond to it. The cause of this pathology is often age-related changes - older cats are usually affected. Another risk factor is obesity.
Type 2 diabetes is the most common - it is diagnosed in 90% of cases.
Third
Type 3 diabetes is called secondary or acquired. Usually its appearance is associated with pathologies of the cat’s pancreas, which arise:
- while taking medications;
- as a consequence of genetic diseases;
- due to metabolic disorders.
This is the mildest form of diabetes in cats. After the underlying disease is cured, the sugar disease will subside.
How is therapy carried out?
When diabetes mellitus is detected in cats, treatment can be quite long and is usually combined. Therapy involves eliminating the factors and symptoms causing the disorder. A prerequisite is the normalization of the animal’s body weight. For this purpose, special dietary foods and a low-carbohydrate diet are used, and insulin-containing medications can also be used.
First aid rules
When a cat is prescribed insulin, it must be injected on a set schedule. Delaying even one injection will disrupt the schedule, which may result in hypoglycemia (excess insulin). The sugar concentration will drop to critical levels, and the cat will show symptoms:
- weakness;
- apathy;
- impaired coordination;
- convulsions;
- coma.
The main thing is to prevent a state of coma, since cats rarely return from it. If you notice these symptoms, it is important to check your sugar levels. If it is critically small, give the animal food with fast carbohydrates. If your cat refuses to eat on his own, pour sugar syrup into his mouth or soak gauze in it and wipe his gums. If the animal does fall into a coma, you should not give it anything to prevent it from choking. It is important to take your cat to the clinic urgently.
Basic therapy
Treatment of cats with diabetes is selected taking into account the form of the disease. If it is the first type, short-acting insulin injections will be needed, and with the second type, instead of hormonal injections, drugs to lower sugar levels or injections of medium or long-term action are required.
- Drugs to reduce sugar. These are mainly tablets prescribed for types 2 and 3 diabetes. The medicine reduces the concentration of sugar to normal levels and eliminates the adverse effects of sugar on all systems and organs. The general condition of the animal is rapidly improving. All medications should be given only as prescribed by a veterinarian, as many have side effects.
- Hormonal injections. The difficulty with using insulin is that it is always difficult to choose a dosage that will help effectively treat the disease. This requires regular glucose monitoring after each new dose. Accordingly, studies are carried out in stationary conditions. The doctor records the time, calculates the dosage and determines the duration of action of insulin injections. Taking into account these data, a scheme for the use of insulin is formed in each individual case.
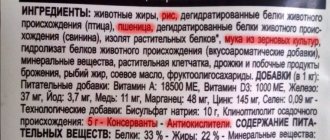
- Correct diet. Normal nutrition for diabetes involves following a diet. A veterinarian should tell you what to feed a cat with diabetes. The main thing is that it is based on animal proteins. At the same time, the volume of carbohydrates is minimized. It is also important to find food without potatoes, cereals, sweeteners and sugar. Meals should be multiple - 5-6 times a day, and always in small portions.
How common is the disease?
No one has conducted studies on the incidence of diabetes mellitus among cats, so there are no official statistics on this issue.
However, it is safe to say that the number of sick animals is steadily growing. This is due to an increase in the number of pet cats that are overweight or obese.
Diabetes mellitus ranks first among endocrine diseases in terms of incidence. Anecdotal evidence suggests that one in 400 domestic cats is diagnosed with diabetes.
Often owners feed their pets and do not care about their physical activity. They are touched by a plump kitten; they do not think about the fact that by the age of 5–6 years he will acquire the status of a diabetic.
Important! In small breed cats, exceeding the standard weight by more than 1.5 kg is considered obese. They will not be allowed to do breeding work, and they will fall into a health risk group.
With age, the likelihood of developing diabetes increases significantly. It is important to pay increased attention to older pets so as not to miss the opportunity to correct their health condition.
The mechanism of pathology development
In a healthy body, glucose is broken down by insulin, converted into energy and nourishes cells. If there is a lack of insulin or immunity to it, glucose does not reach the cells - they starve. As a result, intracellular processes either slow down or stop.
Excess glucose causes the blood to thicken. The cells are instructed to release moisture into the blood to facilitate blood flow. Organ tissues become dehydrated. In order to restore the water balance, a lot of water is needed - the animal becomes thirsty.
The body tries to get rid of excess glucose in the blood and sends it to the kidneys for filtration. “Scared” by a huge amount of sugar, the kidneys are knocked out of the correct mode of operation. The result is increased urination.
If cells do not receive the energy that is generated by the breakdown of glucose, they begin to starve and become exhausted. To prevent the death of the body, the brain switches to “emergency mode”: it commands the cells to break down fat reserves. As a result of the breakdown of fats, ketone bodies enter the blood. This is a by-product of the metabolic process, in other words, poison.
If your cat smells of acetone, the process of ketosis has begun - the formation of ketone bodies. This condition can be corrected with medication and diet. But if measures are not taken in time, ketone bodies will gradually poison the blood and lead to ketoacidosis. Then comes coma and death
Ensuring your cat's well-being
For most cats, stabilization can be achieved very easily with lifelong therapy and related measures. You should work with your veterinarian to determine the best insulin dose, ideal diet, and lifestyle adjustments (if necessary) to achieve maximum control. Make sure you give your cat the correct dose of insulin on schedule. Maintain a regular feeding schedule and offer your pet the amount of food recommended by your veterinarian. Do not give your cat medications, including vitamins or nutritional supplements, without first consulting your veterinarian.
Causes of the disease
Predisposition to diabetes mellitus in cats may be congenital. There are 9 more factors that influence the development of the disease:
- Imbalanced diet. A loving owner wants to pamper his pet and gives him “goodies” from his table. The presence of fatty, spicy, fried, smoked and sweet foods in a cat’s menu leads to overload of the digestive system. The animal's body is not able to cope with such food. This leads to disruption of metabolic processes. The situation is aggravated by non-compliance with the feeding regime.
- Uncontrolled eating will definitely lead to obesity. The cat’s liver and pancreas are forced to constantly work in “emergency” mode. Failures in the functioning of these important organs are inevitable, this serves as an impetus for the development of diabetes mellitus.
- Heart diseases. There are hypertensive cats among cats. The consequence of high blood pressure is disruption of the functioning of many organs. As a result, their sensitivity to insulin decreases.
- Viral diseases. Frequent infections reduce immunity and negatively affect the functioning of internal organs. The pancreas also suffers.
- Acute and chronic pathologies of the gastrointestinal tract. Colitis, ulcers, enteritis, gastritis, pancreatitis can cause the development of diabetes mellitus in cats.
- Congenital pathologies of the pancreas, kidneys, liver, heart.
- Taking diuretics and hormonal drugs to control sexual behavior.
- Stress. Moving, renovations, and frequent visits to pet hotels are good reasons for cat distress. Against the background of a stressful state, eating behavior changes: the cat may refuse food or, conversely, will begin to “eat up” fear. The result is a metabolic disorder, which increases the cat’s chances of acquiring diabetes.
- Lack of physical activity is one of the main factors. Almost all domestic cats exercise little and, as a result, gain excess weight. The animal develops obesity.
Important! Diabetics are most common among castrated and sterilized cats. Males suffer from this disease more often.
Symptoms
Signs that should alert cat owners:
- excessive thirst;
- excessive urination (increased frequency and amount of urine);
- increased appetite or lack thereof;
- dull, sloppy coat;
- tachycardia;
- weight loss.
These are classic signs of diabetes in a cat, so don't hesitate to visit your veterinarian if you notice changes in your pet's condition.
When the condition is neglected, the animal develops wasting of the back muscles, weakness in the hind legs, lethargy, jaundice, convulsions, fainting, the smell of acetone from the mouth, and vomiting.
The cause of the disease can be dry food and Whiskas, so read how to wean your cat off dry food.
Symptoms of diabetes in cats
Depending on the type of diabetes mellitus, the symptoms and clinical picture of the disease look different.
Type 1 diabetes in cats is characterized by increased thirst. Due to insulin deficiency, unbroken sugar enters the blood. The animal's excretory system is not able to process it. The kidneys work harder, resulting in frequent urination.
The cat is thirsty and drinks a lot of water. It turns out to be a vicious circle. Owners may miss the initial manifestations of the disease, since urination does not cause pain to the animal.
Important! If a cat begins to urinate outside the litter box, this is an alarming sign for the owner. It happens that the animal does not have time to wake up in time and partially empties its bladder in its sleep on the bedding.
There may be changes in appetite, the cat's weight increases or decreases greatly. The fur becomes dull and the sick animal sheds constantly. As diabetes develops, digestive system disorders occur - vomiting and diarrhea are possible.
Rapid heartbeat is also a symptom. The cat becomes apathetic and lethargic. At the stage of intoxication of the body, the smell of acetone will appear. This is a sign of liver damage. Convulsions and fainting will complement the list of clinical manifestations.
Animals with type 2 diabetes begin to gain weight sharply. Thirst and frequent urination are noted. The smell of acetone is not noticeable, the appearance of the cat at the beginning of the disease remains the same. As the disease progresses, the quality of vision decreases and lethargy appears. Body itching bothers me. The cat may scratch itself until sores appear.
Type 3 diabetes mellitus is acquired. Its development is directly related to the underlying disease that caused it. As soon as it is eliminated, the sugar disease will go away.
Diagnosis of the disease
Only a veterinarian can make a correct diagnosis of a cat. The symptoms of diabetes in cats and humans are similar, but the treatment methods are different. Only a qualified doctor can prescribe a diet, medications and their dosage.
Typically, an animal does not arrive at a medical facility at the initial stages of the disease. The symptoms are pronounced, but they are also characteristic of many other diseases. Therefore, it is often necessary to carry out differential diagnosis to exclude or confirm concomitant diseases.
When conducting DD, the gastrointestinal tract, liver, and cardiovascular system are examined. Eliminate the presence of parasites and infections.
During a clinical examination, the doctor notes the main symptoms of diabetes mellitus, common to all three types:
- poor condition of the coat;
- exhaustion or obesity;
- change in gait;
- dehydration;
- decrease in body temperature.
Next, the cat’s blood is examined according to the following parameters:
- for sugar content;
- for biochemistry;
- general analysis;
- on thyroid hormones;
A urine sample is required to test for sugar content. The accuracy of the diagnosis will be confirmed by an ultrasound of the abdominal organs.
Forecasts and statistics
A favorable prognosis is typical only for type 3. In other cases, the disease is incurable. Despite this, strict adherence to all medical recommendations makes it possible to stabilize the patient’s condition and prevent relapses. Thanks to proper care, a furry diabetic can live as long as healthy animals.
According to statistics, improvement in well-being is observed even in animals with an advanced form of the disease. But in such situations, veterinarians give a cautious prognosis, since some complications can become an insurmountable obstacle to recovery.
Treatment of diabetes mellitus in cats
Based on the results of tests and examinations, the doctor determines the type of disease and prescribes appropriate treatment. It is necessary to understand that treating diabetes mellitus is a long process. The owner of the animal will need strength, patience, and accuracy.
Treatment is aimed at eliminating either the symptoms of the pathology or the factors that provoked its occurrence.
Insulin therapy
Chronic insulin therapy is necessary for cats with type 1 diabetes. A special drug is produced for them - it differs from the one used to treat people. Insulin therapy is prescribed to the animal depending on the severity of the disease and the phase of the disease. The dosage and dosage regimen is determined by the attending physician individually.
Cat insulin has a short duration of action, so injections will have to be given 2-3 times a day. The injection is placed in the withers with a thin and short needle, so the cat hardly feels pain.
It is strictly not recommended to independently diagnose and treat a cat with insulin. Treatment at home without a doctor's advice will lead to the death of the animal.
If during the initial appointment the doctor suggests leaving the cat in the hospital, you should not refuse. Within 24 hours, the optimal dose of medication for effective treatment will be selected for her. The next day the pet is returned to the owner with precisely verified recommendations.
Diet therapy
Insulin therapy must be combined with diet. For treatment to be successful, the cat’s weight must be brought back to normal. The change in mass should be smooth and gradual.
A clear diet is established. To avoid sudden fluctuations in glucose levels, you should feed your sick cat small meals up to 6 times a day.
Easily digestible carbohydrates are completely excluded from the diet of a diabetic cat. The menu includes protein foods and fiber. Your cat's diet should not include:
- legumes (soybeans, peas, beans);
- flour products;
- porridge - rice, corn, semolina, millet.
Up to 50% of the diet consists of meat and offal, fish, and poultry. They can be given raw, after defrosting. Up to 25–30% comes from lactic acid products – low-fat sour cream and cottage cheese. From 20 to 25% are boiled vegetables.
Specialty stores offer a wide selection of food for diabetic cats. The best premium and holistic medicinal foods:
- Purina Veterinary Diets - normalizes metabolic processes and provides complete nutrition to a sick animal.
- Royal Canin Diabetic - with a high protein content, it contains cereals with a low glycemic index.
The cat owner should understand that a diet is not a temporary measure, but a new way of life for the pet. The basic principles must be followed for life.
Cats at risk for diabetes should not be fed Whiskas brand products - they contain a high amount of carbohydrates.
The prognosis for the results of diabetes treatment is directly dependent on the severity of the cat’s condition at the time of contacting a specialist. At the initial stage, significant investments will be required: both material and resource.
But all these sacrifices pay off. With proper treatment and following all recommendations, the cat’s health will be restored. The life expectancy of a diabetic cat is usually no less than average.
With diabetes mellitus with complications, it is more difficult to give an optimistic prognosis. However, it is worth fighting for the life of a sick pet. Thanks to modern medical technologies and drugs, successful recovery from a diabetic coma, further stabilization of the patient’s condition and long-term remission are possible.
Don't miss the chance to give your pet a few more years of life.
Video
More photos Author(s):
ON THE.
Ignatenko, Ph.D., member of the European Society of Dermatology, member of the European Society of Endocrinology, Kiev, Ukraine / N. Ignatenko, Member of ESVD, ESVE, Kiev, Ukraine Journal:
No. 5 - 2014 UDC 616.379-008.64:636.8 .045
Keywords:
diabetes mellitus in cats, remission of diabetes mellitus, hyperglycemia, hypoglycemia, insulin therapy, diet, exercise
Key words:
diabetes mellitus in cats, remission of diabetes mellitus, hyperglycemia, hypoglycemia, insulin, diet, exercise
annotation
Diabetes mellitus in cats is a common endocrine disorder. The difficulty in recognizing a severe endocrine disorder leads to frequent errors in home therapy for diabetic cats. Five short steps allow you to consistently understand the issues of etiology, clinical manifestations, diagnosis, important aspects of therapy and prognosis of diabetes mellitus, and also facilitate the path to achieving remission, which is the most desirable goal of therapy in diabetic cats.
Summary
Diabetes in cats is a common endocrine disorder. The complexity of perception of severe endocrine disorder resulting in frequent errors in home therapy diabetic cats. Five short stages allow consistently deal with issues of etiology, clinical manifestations, diagnosis, therapy and the important points of the forecast of diabetes. And also make it an easier way to achieve remission, which is the most desirable goal in cats with diabetes.
Diabetes mellitus in cats is a disease that is characterized by a relative or absolute deficiency of insulin and leads to the development of persistent hyperglycemia. It is generally accepted that diabetes mellitus is primarily a problem for old elderly cats, since cats under one year of age are 50 times less likely to develop diabetes mellitus than cats over 10 years of age. Males are more likely than cats to suffer from this disease, but, nevertheless, in the routine practice of a veterinarian, it is becoming more common (if earlier foreign statistics spoke of one case of the disease per 1000 cats, then the modern one indicates that diabetes mellitus may occur in one in 200 cats admitted). Therefore, we can encounter this disease in any age group of any gender and breed and must be prepared to recognize it by its characteristic clinical signs.
1.
Clinical picture
(What is happening to my cat?)
The clinical signs of diabetes mellitus, unlike many endocrine pathologies, are quite characteristic, and we can also count them on the fingers of one hand:
• polydipsia;
• polyuria;
• polyphagia;
• fluctuations in weight;
• in more rare cases with long-term diabetes mellitus - peripheral neuropathy, manifested in a strange plantigrade gait. Cataracts, which are common in diabetic dogs, are not common in diabetic cats. However, it should be remembered that such clinical signs can be observed not only in diabetes mellitus, so it is necessary to carry out a differential diagnosis of disturbing symptoms. We discussed it in detail in No. 4 of the VetPharma-2013 magazine, so I would just like to remind you about hyperthyroidism and chronic renal failure, which are no less rare findings in older cats.
The development of diabetes mellitus in cats is associated with two mechanisms:
1. disruption of the functional state of the beta cells of the pancreas, as a result of which the synthesis and release of insulin and aniline is disrupted;
2. the occurrence of insulin resistance, which leads to impaired utilization of nutrients in tissues sensitive to it. The consequence of these factors is the accumulation of amyloid in the islets of Langerhans; a similar mechanism for the development of type II diabetes mellitus has been described in humans. Just as in humans, one can distinguish between conditionally insulin-dependent, or type I diabetes mellitus, and non-insulin-dependent, or type II diabetes mellitus. As well as transient diabetes mellitus, which can occur against the background of another disease, such as pancreatitis, and go away with effective treatment. Most cats have type II diabetes, but insulin therapy will be a mandatory component of treatment, which we will discuss later.
2. Reasons
(Why is my pet sick?)
There is no one absolute factor that could be called the root cause of diabetes in cats, but it will be easy for owners to name the “top five” among the contributing factors:
• being overweight;
• pancreatitis;
• drug therapy using progestogens and glucocorticoids;
• concomitant diseases: hyperlipidemia, liver diseases, cardiovascular diseases, chronic renal failure, infectious pathology, etc.;
• competitive endocrine disorders (hyperthyroidism, acromegaly).
The importance of genetic predisposition to diabetes mellitus in cats remains controversial. The latter plays a key role in the development of type I diabetes mellitus in humans, but its significance has not been proven in cats.
3. Diagnostics
(How can I be sure that my four-legged family member has diabetes?)
Diabetes mellitus is a rare endocrine pathology, the diagnosis of which is not difficult: for this we only need the triad:
• characteristic clinical signs;
• hyperglycemia (increased blood glucose levels);
• glucosuria (appearance of glucose in the urine).
However, in cats, unlike dogs and people, stress hyperglycemia may occur due to blood collection or other diseases; glucose levels, while normal up to 6.2 mmol/L, can increase to 20 mmol/L. If stress hyperglycemia is so high, then glucose may also appear in the urine (which is unusual for humans and dogs), since with glucose above 10-13 mmol/L in the blood, it will pass through the renal barrier and appear in the urine. Therefore, sometimes, in addition to the listed three components, which in most cases are sufficient, sometimes two more may be needed: determination of glycosylated hemoglobin and fructosamine.
Glycosylated hemoglobin and fructosamine are formed as a result of irreversible nonspecific binding of glucose by amino acid residues. The level of their concentration in the blood is directly proportional to the average concentration of glucose in the blood over a certain period of time, and their content is determined by the overall rate of recycling of the corresponding proteins, which is shorter for serum proteins than for hemoglobin.
Fructosamine is a complex of glycosylated whey proteins, the concentration of which can be determined using a colorimetric assay, which serves as a marker reflecting the average glucose concentration of cats over the past 10-14 days. Glycosylated hemoglobin is a product of the interaction of hemoglobin and glucose, its concentration is determined using chromatography - the concentration in the blood reflects the average level of glucose in the blood over 60-70 days in cats, in contrast to dogs and people, in whom it is considered to reflect the level of glucose over 110 -120 days. Anemia (Ht<35), hypoproteinemia will lead to an underestimation of these indicators, and storing blood samples at room temperature will lead to an overestimation. This must be kept in mind when interpreting indicators. It is worth paying attention to the fact that the levels of glycosylated hemoglobin in cats are significantly lower than in humans ( Table 1
). The cause of lower glycosylated hemoglobin in cats is unknown. It is believed that this is a consequence of the shorter lifespan of red blood cells in cats, different permeability of red blood cell membranes to glucose, or differences in the amino acid composition of hemoglobin in animals of both species, as well as people, which determine the number of glucose binding sites.
4. Therapy
(How to cope with diabetes?)
Once the diagnosis has been made, it is very important to explain to the owner of a diabetic cat that the success of therapy will depend solely on the joint efforts of the doctor and owner, and to strive to achieve maximum mutual understanding. By formulating the goals and objectives that we expect to achieve when starting therapy in diabetic cats, we want not only to eliminate the symptoms of diabetes mellitus, avoid ketoacidosis, as well as other complications and late consequences of diabetes mellitus, but also to achieve remission.
Remission is a decrease in insulin requirements associated with improved function of the remaining beta cells. Partial clinical remission is a significant reduction in the insulin dose (less than 0.4 U/kg per day). Complete clinical remission – no need for exogenous insulin administration. It is assumed that the damaged pancreas in cats, like the liver, is capable of regeneration within 8-12 weeks. Hyperglycemia temporarily suppresses insulin secretion + amyloid deposition leads to the destruction of beta cells. By starting insulin therapy, we remove the factor of the toxic effect of glucose, allowing the pancreas to regenerate. Euglycemia, achieved through insulin therapy + a low-carbohydrate diet 24 hours a day, promotes the regeneration of the pancreas, but tissue resistance to insulin remains for some time. Continuation of therapy leads to a decrease in oxidative stress, a decrease in insulin resistance and a decrease in insulin dosage. Long-term euglycemia leads to recovery of the pancreas. There are high chances of achieving remission in cats with newly diagnosed diabetes mellitus if therapy is quickly started, as long as residual secretion of beta cells is preserved and amyloid deposits in the pancreas are not critical.
The most important components of treating diabetes mellitus in cats in order to achieve remission are:
• insulin therapy started as early as possible;
• intensive monitoring of glucose levels during dose selection;
• high protein diet;
• physical exercise;
• stabilization of other chronic diseases leading to deterioration in the health of diabetic cats.
I would like to dwell on each of these points in a little more detail.
Many cat owners, having heard that their pet has type II diabetes mellitus, try to draw an analogy with people, asking not to prescribe insulin to their animal, fearing that in this way they will suppress the secretion of their own insulin, and simply demand glucose-lowering tablets. But they do not understand the mechanism of action of these drugs, often thinking that this is a different form of release, the so-called insulin tablets. Therefore, at the first appointment, it is very important to explain to the owner that hypoglycemic drugs of all 5 groups that are used in humans (sulfonylureas, thiazolidinediones, meglitinides, biguanides and alpha-glucosidase inhibitors) will not be able to improve the functioning of the pancreas; on the contrary, sooner or later they will lead to her complete exhaustion. While properly selected insulin can help the pancreas recover, if the process is still reversible.
The best drugs for the treatment of diabetes mellitus in cats are long-acting insulin analogues: Lantus, which is recognized as the first choice insulin for diabetic cats, and Levemir, there are still fewer published clinical studies on its use in cats, but the results are also encouraging. Therefore, if the duration of action of Lantus is too short, or there are contrainsular diseases, then it is necessary to try the use of Levemir. Dosing of lantus starts with 0.5 units per kg of body weight of a cat, but not more than 2 units during the first administration. You should start using Levemir in lower dosages: from 0.1-0.2 units per kg.
Insulins are not antibiotics, and their duration of action varies individually: there are patients for whom the drug works for 12 hours, and others for whom it works for 18-24 hours. Less common are cats in which insulin analogues work for 8 hours, and in this case it is necessary to either inject insulin every 8 hours or choose insulin that will work longer. Less effective and with a shorter duration of action in cats are NPH insulins with an intermediate duration of action or mixed insulins, which combine insulin of a short and medium duration of action. With these insulins it is much more difficult to achieve a stable course of diabetes mellitus, and therefore achieve remission.
It is very difficult for the owner of a newly diagnosed diabetic patient to assimilate such large amounts of information at one time, so he needs constant support from the medical staff until he learns to independently grasp the patterns of insulin administration frequency and dosage.
A simpler and more preferable option, at first glance, would be to leave a newly diagnosed diabetic cat in the clinic to determine the dose of insulin and the duration of its action. However, cats in the clinic are under a lot of stress, which can increase stress glycemia, and many of them do not want to eat in the clinic, which also makes dose adjustment difficult. Therefore, if the cat feels clinically well, its appetite is preserved, and there are no clinical and laboratory signs of ketoacidosis or impending hyperosmolar coma, then it is better to adjust the dose of insulin at home.
Before the owner of a diabetic cat picks up a syringe on his own, you must be sure that the owner knows which insulin syringe he needs, and later, when purchasing at the pharmacy, he will choose the right one. Long-acting insulin analogues, such as Lantus and Levemir, are available in syringe pens, 1 step in them is 1 unit, and this is very convenient for dosing, except in cases where the insulin dose is 1.5-2.5, etc. d. Unit In this case, it will be more useful to use insulin syringes with 0.5 or 0.3 U U100 (1 ml - 100 units of active action).
It is also worth remembering that there are different places for injecting insulin in cats, and the skin in the withers area is thicker than the skin in the inguinal fold area. It is important to warn the owner and ask him to practice, under the supervision of a doctor, collecting insulin on his own (this will minimize the likelihood of an insulin overdose) and injecting it (it is important to teach how to inject subcutaneously and not intradermally, since in this case there will be inadequate resorption of insulin, and not intramuscularly, otherwise insulin will be work like short-acting insulin).
After the manipulation (measuring glucose or administering insulin), it is worth rewarding the animal for its good behavior ( Photo 5-9
).
However, when leaving the appointment, the owner must first learn, under the supervision of a specialist, and then independently measure glucose levels. The optimal sites for collection from cats are the ears and paw pads. The latter, however, cannot be called an ideal place for taking blood due to the potential threat of infection in those cats that scoop in the toilet. It is necessary that owners independently in the clinic master simple procedures for drawing blood, observing some small subtleties (warming the ear, applying a drop of Vaseline oil first, using only special lancets for drawing blood, as well as squeezing out a drop with a volume of at least 5 μl to completely fill the capillary test strips), they can easily monitor glucose levels at home and, based on the results, select the dose and time of administration.
It is important to warn the owner that it is necessary to place a cotton pad between the ear and his own finger so as not to pierce his finger, and to press the lancet tightly to the ear.
A drop of blood has been received, now you need to bring a glucometer with a test strip to it to get the result ( Photo 10-14
).
For the first week, so that the owner feels more confident, you can draw insulin into syringes in the clinic, and the owner of the house will only inject it, then the likelihood of an error will be lower. It is very important that when starting insulin therapy, the owner understands that 1 unit and 0.1 ml are not synonymous words! And insulin dosage is never carried out in ml, only in units of active action! When we begin intensive monitoring of a diabetic cat, we aim to restore his pancreas and achieve remission, meaning that as the beta cells recover, the need for exogenous administration will decrease and the insulin dose will need to be lowered. The goal is to achieve indicators of 6-10 (up to 12) in diabetic cats. Because of this, owners may experience episodes of hypoglycemia and must be able to recognize and respond appropriately to them. If the pet owner does not confuse the insulin dose and if the cat eats adequately, then episodes of severe hypoglycemia when using long-acting insulin analogues are rare. But an important message: if a diabetic cat behaves inappropriately: it is too active or, on the contrary, passive, it has an increased appetite or impaired reaction, it staggers or does not respond to stimuli, the first thing is to measure sugar and make sure that the animal does not have hypoglycemia . If the glucose level drops below 4 mmol/l, then it is necessary to urgently feed the animal and repeat the glucose measurement after 30 minutes. If the glucose level is below 3 mmol/l, and the cat has clinical signs of hypoglycemia, then it should immediately lubricate the gums with honey or glucose syrup (while the animal is swallowing) and bring it to the clinic as soon as possible. If a cat has no clinical signs of hypoglycemia, and a medical glucose meter shows less than 2 mmol/l, then this may be due to the fact that humans and animals have different glucose distributions. In humans, the glucose content of red blood cells is 42%, while 58% of glucose is in plasma.
In cats (fewer red blood cells, which are small in size), the glucose content in red blood cells is about 7%, and 93% of glucose is in the blood plasma, so a medical glucometer shows a lower value than it actually is. If the cat is not showing clinical signs of hypoglycemia and the veterinary glucometer shows a glucose level of less than 2 mmol, then it is important to ensure that the capillary of the test strip is completely filled with blood. Incomplete filling of the capillary due to a small drop may lead to an underestimation of the result. In this case, the glucose measurement should be repeated.
If the same dose of insulin begins to work longer over time and reduces glucose levels below 4 mmol/l, then this is one of the signs of approaching remission. It is important not to miss it and to constantly reduce the dose and increase the interval. If glucose is measured only once a day before insulin administration, then it is possible to miss an episode of post-hypoglycemic hyperglycemia and increase the dose when it needs to be reduced. In this case, a chronic increase in dose can lead to the development of insulin resistance - Somogyi syndrome. Characteristic clinical signs of Somogyi syndrome are persistent hyperglycemia with indicators of uncompensated diabetes mellitus against the background of insulin therapy, persistent polydipsia, polyuria, polyphagia and lack of weight loss, and sometimes further weight gain. It is very important to identify this condition promptly (by serially measuring glucose levels every 4 hours) and select the correct dose of insulin.
Cats are obligate carnivores, therefore, for a stable course of diabetes mellitus and achieving remission, it is important to choose a high-protein diet for the animal, in which the protein content will be at least 45%. It is preferable to use wet food. Since most diabetic cats suffer from excess weight, the diet should be aimed at reducing and preventing it. The content of arginine, which increases the secretion of endogenous insulin, is an additional advantage in the direction of high-protein nutrition.
Studies examining the effects of high-protein diets on kidney function have shown that they do not worsen renal function tests (urea, creatinine, phosphorus) in cats or in patients with early-stage chronic renal failure. But it cannot be used in patients with already severe renal failure. It is advisable to feed cats with diabetes twice a day, along with insulin or after its administration. However, there are animals, for example in old age, which are very difficult to retrain to switch to a different type of food. In this case, it is worth trying to give the main portions of food with insulin, and leave a smaller amount of the daily ration for snacks. It is very important not to overfeed a diabetic cat, which is very difficult at the very beginning, with severe symptoms of polyphagia. But excess weight is a factor that not only contributes to the development of diabetes, but also provokes insulin resistance, so it is very important for owners of cats suffering from diabetes to convey the message about the need to reduce excess weight in their pets.
“What to do if insulin doesn’t work?” owners often ask. The most important reason for the ineffective action of insulin is the owner of the animal, so first of all it is necessary to check the accuracy of the dose, the correct administration and storage conditions of the insulin. If everything is done correctly, then try to change the dose. If a cat receives more than 2 units per kg of lantus or levemir, and glucose levels remain high, then we are talking about insulin resistance and should try to find out its causes. Of the endocrine disorders, antagonistic diseases can primarily be hyperthyroidism and acromegaly; hyperadrenocorticism is very rare in cats. But even such routine diseases as asymptomatic chronic cystitis can cause insulin resistance, so at the stage of the first clinical studies it is important to create the most complete overall picture of the health of a cat suffering from diabetes.
In addition to the correct dose selection of long-acting insulin analogues and high-protein nutrition, it is very important to get the cat moving. Physical activity is also a necessary moment in increasing tissue sensitivity to insulin. Therefore, it is important to discuss with the owners all the possibilities of how to make the cat move more: you can put food little by little in different parts of the kitchen, buy toys in which you can pour food inside, and the cat will require physical effort in order to get it, from running after a laser pointer to catching virtual fish on a tablet - all means are good.
5. Forecast
(How long will my pet live after he gets diabetes?)
The prognosis for any diabetic animal is unpredictable. Much depends on the owner (degree of affection, willingness to devote time to treating and monitoring the pet), the presence and severity of concomitant disease. According to statistics from foreign authors, 50% of cats diagnosed with diabetes mellitus die within 12-17 months after diagnosis (including aggravating diseases). Nelson writes: “... cats that survive the first 6 months after diagnosis of diabetes mellitus maintain a good quality of life for more than 5 years, despite the disease...”
The owner must remember that weight loss helps to lengthen life expectancy. Modern sources are more optimistic about the life expectancy of diabetic cats: the median is 516 days. And, in my opinion, these indicators will improve as intensive home monitoring and therapy with long-acting insulin analogues improve. Early initiation of insulin therapy helps achieve remission in 70-80% of cats with newly diagnosed diabetes mellitus. The prognosis is worsened by chronic renal failure, as well as previous ketoacidotic or hyperosolar coma. But more about this in the next issues of the magazine.
Literature
1. Kirk R., Bonagura D. Kirk’s modern course of veterinary medicine. – M.: Aquarium-Print, 2005, – 1370.
2. Pibo P., Burge V., Elliott D. Encyclopedia of clinical nutrition for cats. – M.: Media Line, 2009, – 518 p.
3. Torrance E.D., Mooney K.T. Guide to small animal endocrinology. – M.: Aquarium-Print, 2006, – 312 p.
4. Feldman E., Nelson R. Endocrinology and reproduction of dogs and cats / ed. A.V. Tkacheva-Kuzmina and others - M.: Sofion, 2008 - 1242 p.
5. Astrid Wehner. Diabetus meltus bei Hunde und Katze. EndokrinoLogie SS 2009 lectures for students of MTK LMU, Muenchen.
6. Connally HE Clin Tech Small Anim Pract. May 2002; 17(2):73-8. Critical care monitoring considerations for the diabetic patient.
7. Diabetic emergencies in small animals. O'Brien MA. Source Department of Veterinary Clinical Medicine, University of Illinois at Urbana-Champaign, 1008 West Hazelwood Drive, Urbana, IL 61802, USA.
8. Evaluation of detemir in diabetic cats managed with a protocol for intensive blood glucose control. Roomp K., Rand J. https://www.ncbi.nlm.nih.gov/
pubmed/22553309.
9. Gilor C., Graves TK Vet Clin North Am Small Anim Pract. Mar 2010; 40(2):297-307. doi: 10.1016/j. cvsm.2009.11.001. Synthetic insulin analogs and their use in dogs and cats.
10. J Diabetes Sci Technol. 2012 May 1; 6(3):491-5. Monitoring methods for dogs and cats with diabetes mellitus.
11. Laflamme DP. J Anim Sci. May 2012; 90(5):1653-62. doi: 10.2527/jas.2011-4571. Epub 2011 Oct 7. Companion Animals Symposium: Obesity in dogs and cats: What is wrong with being fat?
12. Plotnick AN, Greco DS Home management of cats and dogs with diabetes mellitus. Common questions asked by veterinarians and clients Nichols R. Semin Vet Med Surg (Small Anim). 1997 Nov; 12(4):263-7.
13. Predictors of clinical remission in cats with diabetes mellitus. Zini E., Hafner M., Osto M., Franchini M., Ackermann M., Lutz T.A., Reusch C.E. https://www.ncbi.nlm.nih.gov/pubmed/20840299
14. Rock M., Babinec P.. Diabetes in people, cats, and dogs: biomedicine and manifold ontologies. Vet ClinNorth Am Small Anim Pract. May 1995; 25(3):753.
15. Wiedmeyer CE, DeClue AE Clin Lab Med. Mar 2011; 31(1):41-50. doi: 10.1016/j.cll.2010.10.010. Epub 2010 Nov 24. Glucose monitoring in diabetic dogs and cats: adapting new technology for home and hospital care. Vet Clin North Am Small Anim Pract. Mar 2010; 40(2):317-33. doi: 10.1016/j.cvsm.2009.10.003.
16. Zini E., Osto M., Franchini M., Guscetti F., Donath MY, Perren A., Heller RS, Linscheid P., Bouwman M., Ackermann M., Lutz TA, Reusch CE Hyperglycaemia but not hyperlipidaemia causes beta cell dysfunction and beta cell loss in the domestic cat.
https://www.ncbi.nlm.nih.gov/pubmed/19034421. Back to section
Treatment control
Throughout the entire period of treatment for diabetes, it is necessary to monitor the blood sugar level of a sick cat. This can be done using a glucometer. The owner keeps a special journal in which he records the dosage and time of injection, as well as the date, time and device readings.
Using these records it will be convenient to track the dynamics of treatment.
Even after recovery, you need to regularly monitor your sugar levels. In order not to expose your cat to unnecessary worries when visiting the clinic, you can purchase special test strips. They are sold in every veterinary pharmacy.
Expert opinion
Chepa Natalya Semenovna
Veterinarian
Ask a Question
Among cats, fold-eared breeds are most prone to otitis, because... they have a small closed ear and a narrow ear canal that is poorly ventilated. Hairless breeds produce a lot of sulfur, which can also be a predisposing factor for the development of otitis media. A common mistake owners make when caring for their ears is using a cotton swab. It will not be possible to clean the ear well with a cotton swab due to its structure, but leaving the cotton swab, “compacting” the wax inside the passage and causing irritation of the skin of the ear canal is quite likely. For home care, it is best to use special lotions no more than once a month. You should not use multi-component ear drops on your own. Medications should be prescribed by a doctor based on a cytological examination.
Why therapy doesn't help
It happens that prescribed therapy does not bring the expected result.
Example: A cat has been diagnosed with all the characteristic manifestations of diabetes mellitus. Insulin therapy was prescribed, but the animal's condition worsened.
Blood sugar in cats can normally be slightly elevated. When experiencing stress, elevated levels of glucose in the blood and urine can persist for a long time. Also, too “sweet” urine is detected in some inflammatory and infectious diseases of the kidneys. This symptom is also characteristic of lymphoma.
In this case, inadequate treatment was provided due to an incorrect diagnosis.
In treatment, a lot depends on the cat’s owner. Negligence in performing the necessary procedures, untimely injections, non-compliance with medication dosages will affect the quality of therapy.
List of complications and dangerous conditions
The disease is rarely complicated by concomitant diseases at an early stage. Most often they appear only after a few years and include:
- cystitis;
- heart pathologies;
- cataract and retinopathy;
- liver and kidney failure;
- ketoacidosis;
- diabetic neuropathy and angiopathy;
- trophic ulcers;
- hypoglycemia;
- deformation and thinning of bones.
You should not wait for these complications to appear, since delayed treatment does not always produce results. If there are any signs of illness, take your pet to the veterinary clinic and wait for the veterinarian's conclusion.
Complications of diabetes in cats
Any advanced disease leads to complications that affect vital organs. Diabetes mellitus is no exception and can lead to irreversible functional impairment.
Ketoacidosis
In diabetic ketoacidosis, there is an increased content of ketone bodies in the blood. This indicates a metabolic disorder: the liver cannot cope with its work and begins to poison the body.
It is difficult to make a mistake with the diagnosis: the cat smells of acetone, it develops shortness of breath, and cardiac dysfunction. If it is not too late to see a doctor, drug treatment will help save life.
Diabetic neuropathy
When the level of glucose in a cat's blood exceeds, damage to peripheral nerve endings is observed. As a result, weakness of the hind limbs develops. When diagnosed, unsteadiness and uncertainty of gait are noted. A sick cat's paws are noticeably cooler than its body.
Hypoglycemia and hypokalemia
Hypoglycemia is a sharp decrease in blood glucose levels. Characteristic features:
- excitement, anxiety is replaced by lethargy and drowsiness;
- muscle tremors;
- impaired coordination of movements;
- unsteady gait;
- fainting.
To bring a cat out of a state of hypoglycemia, you need to pour a strong solution of sugar or honey into its mouth. Then you need to contact a veterinarian.
Hypokalemia is a critical decrease in potassium levels in the blood. This is a consequence of frequent urination - potassium is excreted in the urine. The condition often occurs when a cat is treated with insulin and is manifested by the following symptoms:
- diarrhea;
- vomit;
- acute heart failure.
The cat may die; you need to urgently take it to the veterinary clinic.
Hypoglycemia and hypokalemia are life-threatening, but with timely medical care, a sick animal can be saved. With appropriate treatment and diet, it is quite possible to provide a comfortable life for your cat.
Possible complications
The pathology is dangerous with severe complications. Elevated glucose concentrations have a detrimental effect on health. Among the most common consequences that diabetes leads to is, first of all, ketoacidosis, which can result in the death of a four-legged pet.
Infusion and insulin therapy can save him, but you need to act quickly. Other complications include diabetic neuropathy, hypoglycemia, hypokalemia, which also often lead to death.