Victoria Rashidovna Khazimulina
veterinarian Petstory
Our pets have to deal with such pathology as gastritis in cats. This disease is characterized by an inflammatory process of the stomach wall. Unfortunately, the first symptoms of gastritis can be mild; the pet often comes to the doctor at an advanced stage, when vomiting has begun or appetite has decreased. This happens because cats are very patient animals and it is difficult to tell if they are experiencing discomfort or pain. Therefore, it is very important to know how to recognize the signs of the disease, how to properly help your pet, how to treat gastritis in a cat, and how to prevent this disease in the future.
Types of gastritis
Gastritis in cats has different classifications. He can be:
- Acute or chronic, depending on the duration of the disease and the severity of symptoms;
- Primary (independent disease) or secondary (as a complication of other pathologies);
- Diffuse (the entire wall of the stomach is affected) or focal (a specific area of the organ is affected);
- Hemorrhagic (with bleeding of the inner wall of the stomach);
- Erosive (with the formation of erosions);
- Ulcerative (with the formation of ulcers);
- Necrotic (with tissue death), etc.
How to help at home?
Treatment of gastritis in cats at home is carried out in compliance with basic methods of therapy. In the absence of medicinal food, exclude all ready-made meals, sausages and milk from the cat’s diet. River and sea fish with lots of bones should not be given.
You can feed your cat raw or boiled good quality meat, without fat and bones (beef, chicken, turkey). Cat food may contain low-fat fermented milk products (sugar-free yogurt, kefir). Feed 6-8 times a day, giving little food at a time, even if the cat is ready to eat more. You can additionally give your domestic cat fresh young grass.
To reduce stomach pain, give coating agents and antacids (Phosphalugel, Almagel) before meals. The dosage is 0.5-1 ml per 1 kg of weight. It is convenient to dose and water the animal using a syringe without a needle. In the absence of medications, a slimy decoction of rice or oatmeal, brought to the consistency of liquid jelly, is suitable. The dosage is the same.
All information posted on the site is provided in accordance with the User Agreement and is not a direct instruction to action. We strongly recommend that before using any product, you must obtain a face-to-face consultation at an accredited veterinary clinic.
Causes of the disease:
- Errors in feeding. An unbalanced diet, a high content of difficult-to-digest foods (table foods, excess spices, fried foods), stale foods (spoiled food, leftover food from the trash or on the street), too cold or hot food, a sudden change in diet, overeating;
- Food intolerance (allergic and non-allergic);
- Infections;
- Taking medications. Long-term use of drugs from the group of corticosteroids and NSAIDs can provoke the development of gastritis. Some human drugs from the NSAID group are contraindicated in animals even for single use (for example, ketorol, ibuprofen, diclofenac, indomethacin, paracetamol, etc.);
- Complication of other diseases. Gastritis in cats often occurs in combination with other gastrointestinal diseases (gastroenterocolitis, IBD, pancreatitis, cholecystitis, etc.). It can also develop against the background of many systemic diseases (CKD, hyperthyroidism, diabetes, stomatitis);
- Helminths and protozoa;
- Foreign objects in the stomach. Wool, accidentally eaten food packaging, threads, pieces of toys, hair ties;
- Stress. Some cats refuse to eat due to stress, which is dangerous to their health;
- Poisoning. Road reagents, household chemicals, pesticides, building materials, cosmetics, various plants. Do not forget that the cat is constantly licking itself, and if it gets dirty (for example, in paint), it will lick it off;
- Neoplasms. Tumors can occur both in the stomach itself and in neighboring organs;
- Secretion disorders. They can be either congenital or due to other diseases or when taking certain medications.
Development mechanism
There are two options involved. The first is when a hungry cat begins to secrete gastric juice (hydrochloric acid) at the sight of food. If the situation is repeated frequently, it provokes inflammation of the gastric mucosa.
In the second case, the disease develops in a well-fed pet when the breeder overfeeds it. Less gastric juice is secreted, the food remains stale, which is fraught with the development of inflammation of the mucous membrane and putrefactive processes.
A separate issue is uremic gastritis, which develops against the background of impaired renal function. More often, with nephritis, ICD, the excretory system begins to work incorrectly, and urea levels in the blood increase. It is this substance that is released through the gastric mucosa, the secretory and motor functions are disrupted, and inflammation develops.
Symptoms of gastritis in cats
Gastritis in cats can manifest itself in different ways. Symptoms to watch out for are:
- Oppression. The first sign may be a decrease in activity, attempts to hide in secluded places, refusal to play;
- Decreased quality of skin and coat. The coat is dull and disheveled;
- Change in appetite. Decreased rate of eating or volume of food eaten;
- Bad breath;
- Weight loss, weight loss;
- Increased salivation, frequent swallowing (symptom of nausea);
- Vomit. In a chronic course, the symptom may appear or resolve on its own;
- Pain. The pet moves carefully and slowly, hunches over, searches for a comfortable position for a long time, meows more often, and its belly is hard. The pain may not be acute or may occur intermittently, then the pet will either show signs of pain or behave as usual;
- Changing the stool. Gastritis can cause both diarrhea and constipation. It is also worth paying attention to the volume and color of the stool. Normal stool is brown. If you notice that the stool has become black, green, white, or the volume of the stool has increased, you should consult a doctor.
Stomach diseases of dogs and cats
The stomach in cats and dogs is an independent organ that is part of the digestive tract. Like any organ, the stomach is susceptible to specific diseases, each of which has its own name, etiology and pathogenesis. One of the most important tasks of a clinician faced with a stomach disease is to determine which particular nosological unit he is dealing with, since both the diagnostic plan and the tactics of further treatment depend on this.
Typically, gastric disease results from inflammation, ulceration, neoplasia, or obstruction. The clinical manifestations of stomach diseases are similar: most often it is vomiting and/or retching, hematemesis, melena, belching, hypersalivation, abdominal discomfort, weight loss (in chronic diseases). Gastritis, which will be discussed in this material, is only a part of the many diseases associated directly with the stomach. Most often, veterinarians deal with the following stomach pathologies:
- inflammation (gastritis)
- acute dilatation
- volvulus
- erosions and ulcers
- neoplasia
- motor disorders
Gastritis is one of the most frequently diagnosed diagnoses when a patient is admitted with a complaint of acute or chronic vomiting. Meanwhile, acute/chronic vomiting syndrome is extremely common in small animals and in the vast majority of cases has many other causes. A clear understanding of the cases in which the diagnosis of “gastritis” is legitimate is necessary. In addition, since acute/chronic vomiting syndrome can occur for a variety of reasons, and making a diagnosis in this case is not an easy task, it is very important to follow a generally accepted diagnostic plan to avoid errors in diagnosis and, subsequently, in the treatment of the patient.
Stomach - structure and functions.
The stomach consists of 4 functional sections: cardia, fundus, body and antrum.
- the cardiac section is responsible for controlling the flow of food from the esophagus into the stomach (and the esophageal sphincter prevents it from flowing back into the esophagus)
- the body and fundus of the stomach have a high ability to stretch (ingesting a large volume of food)
- the antrum has a thicker muscle wall (grinding and homogenization of the food mass before entering the intestine)
- The pyloric sphincter controls the flow of chyme into the intestines
The histological structure of the stomach corresponds to that of any tubular organ (see diagram below). The gastric epithelium is secretory and produces both a protective buffer for the mucous membrane and digestive enzymes (the type of secretion depends on the location of the epithelium in the sections of the stomach).
Schematic diagram of the structure of a tubular organ, from the site https://www.vetmed.vt.edu
The author recommends this online resource as a real storehouse of educational information with very accessible explanations, drawings and microphotographs
Digestion of nutrients.
Gastric juice helps begin the digestion of proteins (pepsin) and fats (gastric lipase), and also stimulates gastric emptying and stimulation of the secretory function of the pancreas. In addition, gastric acid limits the proliferation of gastrointestinal microflora. It is noteworthy that gastric lipase remains active in the small intestine and accounts for up to 30% of total lipase in dogs.
The stomach is protected from gastric acid by the BSG - a barrier of the gastric mucosa. This concept includes a dense epithelial layer, secreted bicarbonate mucus, local production of prostaglandins and rapid repair of the epithelium in case of damage.
Microflora of the stomach.
The stomachs of dogs and cats are constantly inhabited by Helicobacter spp. These are acid-tolerant microorganisms that produce urease to create a buffer that protects them from acid. Some other bacteria (Proteus, Streptococcus, etc.) may be temporarily present, but normally acid secretion and normal peristalsis successfully regulate their numbers. Therefore, with a decrease in the secretory function of the mucosa, proliferation of these microorganisms may be observed. The role of Helicobacter in the development of inflammation and mucosal atrophy in cats and dogs is debated.
The diagnosis of “gastritis” is one of the most common diagnoses made by veterinarians for animals whose owners complain of acute or chronic vomiting. Meanwhile, the syndrome of acute (chronic) vomiting is not always associated directly with the gastrointestinal tract, and stomach diseases are not only gastritis. In addition to inflammatory causes, stomach diseases can be associated with a number of others. In foreign literature, stomach diseases are usually divided according to their etiology and pathogenetic mechanism:
- inflammation
- infectious (invasive) causes (infection)
- diseases associated with obstruction
- diseases associated with impaired motor skills (dysmotility)
- oncological diseases (neoplasia)
- erosive and ulcerative lesions (ulcer)
In this article we will consider only one group of diseases united by inflammation as the main pathogenetic mechanism of development.
Acute gastritis.
Acute gastritis is the term used to define the syndrome of sudden onset of vomiting. Most often, the cause of the condition can be determined by questioning the owner in detail. Damage to the gastric mucosa with subsequent inflammation can occur either through direct contact with a damaging substance (in this case we are talking about primary acute gastritis), or due to indirect damage associated with diseases of other organ systems (secondary gastritis, a striking example is uremic gastropathy in chronic renal failure).
Clinical signs.
The main clinical sign is sudden onset of vomiting. It is important to remember that sometimes anorexia may be the only clinical sign (as a consequence of nausea) in acute gastritis. The general condition of the animal is most often satisfactory; there may be a decrease in appetite and activity. If acute gastritis is associated with the ingestion of foreign bodies, toxins, systemic disorders, there is often an admixture of blood in the vomit, feces, concomitant diarrhea, and a significant deterioration in the general condition. Such patients require a more thorough diagnostic approach.
Diagnostics.
Based on anamnestic data, clinical manifestations and response to symptomatic treatment. If there is no evidence of systemic disease, diagnostic testing is usually not necessary. However, it is necessary to begin the examination immediately if:
- there are signs of a systemic disease;
- there is a significant deterioration in general condition;
- in addition to vomiting, there is diarrhea, abdominal pain, blood in the vomit and/or stool
- fever is present
- history of eating foreign objects, toxic substances;
- no response to symptomatic therapy within 1-2 days.
The basic diagnostic profile in these situations includes:
- general clinical and biochemical blood test, stool test for parasites (flotation method), urine test
- X-ray examination (with and/or without contrast)
- Ultrasound
- endoscopy
Additional studies may be included in the examination protocol based on the results of basic tests (PCR for infections, bile acid test, test for specific pancreatic lipase, etc.)
Treatment.
For uncomplicated acute gastritis, treatment is most often symptomatic. If the cause of the condition is known, the first step is to eliminate it, if possible.
Diet therapy.
It is advisable to provide “rest” to an inflamed stomach. Its duration depends on the age of the animal and the severity of gastritis. The fasting diet should not be too long, since the flow of food into the gastrointestinal tract maintains its barrier function. Usually for uncomplicated gastritis it is 12-24 hours. The inflamed mucous membrane reacts to stretching, so to avoid resumption of vomiting, portions of water and food should be as small as possible. The main goals are to avoid stretching the stomach walls and minimally stimulate acid secretion. It is known that among protein sources, the most active secretion stimulator is animal protein, and vegetable and milk proteins stimulate acid production the least. Therefore, when choosing a diet for a patient who is on a natural diet, it is worth choosing low-fat cottage cheese and rice in a ratio of 1:3. Of the ready-made diets, the best options are those containing soy hydrolysate as the only source of protein (for example, Purina® HA), or easily digestible therapeutic diets with a low protein content for animals with gastrointestinal diseases (for example, Purina® EN).
Infusion therapy.
In uncomplicated acute gastritis, fluid loss is rarely significant, although in small animals repeated vomiting can cause dehydration. If the fluid deficit is less than 5%, subcutaneous administration of isotonic solutions is effective. If significant dehydration occurs, intravenous infusions are required and such animals should be monitored and examined more closely.
Gastroprotectors.
Drugs in this group are prescribed for gastritis to protect the gastric mucosa, as well as to bind bacterial toxins and the bacteria themselves. The drugs of choice are:
- sucralfate (dogs 1 g/30kg every 8-12 hours, 30-60 minutes before feeding, cats 250 mg/cat); You can prepare a suspension from the tablet form and drink it, this is considered more effective.
- Bismuth preparations: have a cytoprotective effect and are also active against Helicobacter bacteria. Long-term use should be avoided due to possible adsorption of bismuth salts.
H2-blockers and antibiotics: it is advisable to prescribe them in case of signs of erosive damage to the gastric mucosa (hematemesis, melena), as well as in chronic gastritis. For acute uncomplicated gastritis, they are usually not necessary.
Antiemetics.
The prescription of antiemetic drugs for acute gastritis is justified only in cases where intense repeated vomiting leads to significant dehydration and significantly worsens the animal’s condition. In other cases, it is worth trying not to prescribe antiemetic drugs in order to assess the response to symptomatic treatment (diet therapy + gastroprotectors). If vomiting continues, antiemetics are included in the treatment protocol and the diagnostic plan is revised. Drugs of choice:
- maropitant 0.1 ml/kg once a day; in addition to a powerful antiemetic effect, it significantly reduces abdominal discomfort, which can significantly improve the patient’s general condition in a short time.
- metoclopramide 0.2-0.5 mg/kg every 8-12 hours; The antiemetic effect is weaker than that of maropitant, but its prokinetic effect suppresses gastroesophageal reflux and promotes gastric emptying.
Chronic gastritis.
This is a fairly common disease in dogs (found on average in 30-35% of dogs examined both for chronic vomiting and for other reasons; characteristic symptoms may not be expressed); There are no reliable studies on the incidence of chronic gastritis in cats. Important aspects:
- chronic gastritis is a histological diagnosis, that is, it can only be confirmed by histological examination of gastric biopsies;
- all possible causes of chronic vomiting must be excluded before a diagnosis of chronic gastritis can be made;
- If the diagnosis of chronic gastritis is confirmed histologically, it is necessary to try to find its cause before recognizing it as idiopathic. Most often, the cause can be identified.
The causes of chronic gastritis can be the same factors as in acute inflammation (see table). If these factors are absent, chronic gastritis is associated with food allergies or food intolerance, a hidden parasitic disease, a reaction to bacterial antigens (including the gastrointestinal tract's own microflora).
Gastritis in dogs and cats is classified by histopathologists according to the following histological changes:
- the predominant type of infiltrating cells (eosinophils, lymphocytes, plasma cells, etc.)
- structural changes (atrophy, hypertrophy, fibrosis, etc.)
- degree of severity – subjective (mild, moderate, severe)
Histopathological assessment of biopsies is not standardized for dogs and cats, so much depends on the experience and qualifications of the histopathologist. Care must be taken when selecting a laboratory to send samples to, as medical evaluation standards differ significantly from those for animals, and it is not uncommon to receive confusing results when relying on the opinions of medical professionals.
The most common type is superficial lymphoplasmacytic gastritis of mild or moderate severity with concomitant lymphoid follicular hyperplasia .
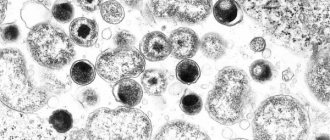
Photo from https://scialert.net
Picture of chronic lymphoplasmacytic gastritis. Wide arrows indicate areas of lymphoid follicular hyperplasia
Clinical symptoms.
The main symptom is chronic vomiting of food or bile. There may be periods of spontaneous improvement and worsening, or chronic vomiting may occur with the same frequency. Decreased appetite, weight loss, hematemesis, and sometimes melena may be present. Associated skin lesions and/or stool abnormalities increase the likelihood of a food allergy. Physical examination usually does not reveal any significant changes.
Diagnostics.
The results of standard laboratory tests (clinical and biochemical tests of blood, urine, X-ray examination, ultrasound), as a rule, do not have characteristic changes in chronic gastritis, but they should always be carried out to try to exclude systemic or metabolic or other problems not directly related to the stomach cause of chronic vomiting. Detected eosinophilia may indicate the presence of gastritis associated with parasites or food allergies, mastocytoma. Panhypoproteinemia is observed in generalized IBD (IBD), gastrointestinal lymphoma, and Norwegian Lundehund gastroenteropathy. High levels of globulin and low levels of albumin can be observed in Basenjis with gastroenteropathy characteristic of this breed.
Endoscopic examination with biopsy samples.
It is a key study for the final diagnosis of chronic gastritis. Biopsy samples should be taken even when macroscopic assessment of the mucous membrane does not reveal visual changes. The result of histological examination is extremely important from the point of view of choosing treatment tactics, since with different degrees of severity of the same form of gastritis, different treatment regimens will be used.
Idiopathic chronic gastritis
If all possible systemic/metabolic/endocrine causes of gastritis have been excluded at the stage of the standard examination protocol, chronic gastritis, confirmed histologically, is recognized as an idiopathic form (that is, a disease whose etiology is not clear). The most common type of idiopathic chronic gastritis in cats and dogs is mild to moderate lymphocytic-plasmacytic gastritis. This term means that the gastric mucosa is infiltrated (“impregnated”) with inflammatory cells – lymphocytes and plasmacytes. This process may be accompanied by atrophy and fibrosis of the mucosa, and less often by hyperplasia.
Mild lymphoplasmacytic gastritis.
The most common option, and the first stage of treatment, usually involves prescribing an elimination diet containing a new source of protein for the animal. If the patient receives a natural diet, the diets recommended for dermatological patients (fish and potatoes for dogs, pork or horse meat for cats) can be used as the basis for therapeutic feeding. The diet of animals kept on ready-made diets is easier to adjust. For dogs, you can use Purina® Veterinary Diets DRM, which contains capelin as the main protein source, or Purina® Veterinary Diets HA, which contains hydrolyzed soy protein as the only protein source. For cats, the NA diet for cats is suitable.
In addition to being a preferred source of protein, these diets also contain sufficient amounts of polyunsaturated fatty acids and antioxidants, which are likely to reduce mucosal inflammation. Sufficient carbohydrate and fiber content will contribute to timely emptying of the stomach.
In gastroenterology, an elimination diet is prescribed, in contrast to dermatological regimens, for 2 weeks - this is how long it takes to evaluate its effectiveness, in addition, this is usually the maximum period that the patient’s owner agrees to. If the diet has proven to be effective, challenge tests with components of the original diet can be performed to identify the product causing vomiting. Practice shows that owners often refuse provocative tests, in which case the patient can be left on an elimination diet. You can try another diet option if the first one turns out to be ineffective, but most often in these cases you have to switch to drug therapy, since vomiting that continues despite the treatment started bothers both the patient and its owner. The drug of choice is prednisolone, it is prescribed orally at a dose of 1-2 mg/kg 1 time per day, after vomiting stops, the dose is reduced to 1 time per 48 hours, then the dose is gradually reduced to the lowest level that maintains remission (the dose is reduced until vomiting starts again , then you need to return to the previous effective dose and stay on it for about 8-12 weeks).
Moderate to severe lymphoplasmacytic gastritis.
Treatment with prednisone begins immediately, always combining it with an elimination diet. After vomiting stops, the dose of prednisolone is reduced, as in the previous case, and the diet is left for as long as possible. Moderate and severe degrees of LPG are often combined with the formation of erosions and even ulcerations of the mucous membrane; in these cases, gastroprotectors and H2 blockers are included in the treatment regimen:
- orally Sucralfate 1 g/30 kg one hour before feeding to dogs 2-3 times a day, 250 mg/cat in the same regimen;
- orally, intravenously Famotidine 0.1-0.5 mg/kg 2 times a day.
Long-term administration of antisecretory drugs (H2-blockers, proton pump inhibitors) should be avoided, since in this case excessive growth of gastric flora is possible, as well as the development of hypertrophic gastritis (not yet confirmed in cats and dogs).
If there is no improvement with diet, prednisolone and gastroprotectors, you should reconsider the diagnosis before starting more aggressive immunosuppressive therapy and make sure that all metabolic/systemic/endocrine causes of the development of chronic gastritis are excluded.
If it is still necessary to use drugs with a more pronounced immunosuppressive effect, or if the patient has a significant side effect of prednisolone, the drug of choice for dogs is azathioprine (orally 2 mg/kg once a day for 5 days, then alternates with prednisolone, azathioprine for 1 day , 1 day prednisolone). For cats, the drug of choice is chlorambucil at a dose of 0.25 mg/kg every 24-48 hours.
Eosinophilic gastritis.
Clinical signs are similar to those of lymphoplasmacytic gastritis; histologically manifested in infiltration of the gastric mucosa by eosinophils (or eosinophils will predominate in the cellular infiltrate). Most often, this type of gastritis is associated with hypersensitivity to food components or with endoparasitosis, therefore, before starting immunosuppressive therapy, it is necessary to carry out deworming, even if parasites were not detected in fecal samples. In general, treatment tactics for eosinophilic gastritis are identical: elimination diet, immunosuppressants, gastroprotective agents for moderate and severe inflammation.
Other forms of chronic gastritis (histiocytic, atrophic, hypertrophic, etc.) are rare in cats and dogs and are most often associated either with specific lesions (for example, infection with a fungus of the genus Pythium in histiocytic/granulomatous gastritis), or with a breed predisposition to certain gastropathy (for example, hypertrophy of the antral mucosa in dogs of brachycephalic breeds - Lhasa Apso, etc. This can lead to obstruction of the pyloric part of the stomach and requires surgical correction)
From the site https://www.familyvet.com
Hypertrophic gastritis and pyloric hypertrophy of the mucosa in brachycephalic dogs.
Summary:
Gastritis in dogs and cats is a common disease.
Acute gastritis is the term that defines the syndrome of acute vomiting. Primary uncomplicated acute gastritis is a diagnosis made on the basis of anamnestic data, physical examination and response to symptomatic treatment; examination is usually not required. The prognosis is favorable.
Chronic gastritis is largely a histological diagnosis, which can only be confirmed by histopathological examination of gastric biopsies.
Careful exclusion of possible systemic/metabolic/endocrine causes is necessary before chronic gastritis can be considered idiopathic. Often the root cause is found, and in some cases it can be eliminated.
It is not possible to establish the cause of the idiopathic form of chronic gastritis; treatment tactics are based on the premise that this is an immune-mediated process. The prognosis of the disease depends on the severity and response to specific therapy.
Article on our Yandex Zen channel.
Diagnostics
- Doctor visit. He will take a detailed history and conduct a thorough examination;
- Ultrasound of the abdominal cavity;
- Blood tests. It is important to mention that there is no specific indicator that specifically indicates inflammation of the stomach. However, blood tests are needed to identify concomitant pathologies (pathologies of the kidneys, liver, pancreas, etc.);
- Gastroscopy . The procedure is performed under sedation and is a very informative research method. During the examination, you can immediately take material from the wall of the stomach or remove a foreign object;
- Biopsy. Required in some cases, in case of severe long-term gastritis or suspected tumor processes;
- X-ray with contrast agents. It is required in some cases to assess the patency of the gastrointestinal tract, the presence of dilatations, diverticula, and foreign objects.
What to feed a cat with gastritis?
The most important thing is easily digestible ingredients, fractional feeding, warm food, wet diets. Split feeding is recommended, every 2-4 hours.
If your pet is accustomed to industrial diets, then you need to switch it to special food with protein hydrolysate. Protein in such diets is absorbed much easier and, accordingly, does not linger in the stomach and intestines, and also does not provoke food rotting processes.
What to feed a cat with gastritis if he is used to eating diets prepared at home? It is important to give preference to proteins high in arginine, glutamine, glycine and lysine (seafood, eggs, cottage cheese). If a food intolerance is suspected, an elimination diet may be recommended, meaning that only one source of protein will need to be maintained. Regarding carbohydrates, you need to limit the intake of non-fermentable fiber; the carbohydrates themselves should also be easily digestible (corn, rice, wheat, barley). Fats in the diet should be limited as much as possible. And fill the daily need for fats with saturated fats (fish oil, sunflower oil, avocado).
Natural products
To begin with, it is worth clearly indicating that natural products are those that are prepared specifically for the cat, and not those that are left on our plate after dinner. They should not contain seasonings, oil, marinades, or mayonnaise.
Natural feeding of a cat means excluding fatty, fried, smoked foods, because this is what leads to gastritis.
Products included in the diet for gastritis
An “undesirable” product will provoke an exacerbation of gastritis, diarrhea or vomiting. This can significantly aggravate the situation and worsen the pet’s well-being.
It is very important to adhere to the list of permitted products, which includes:
- boiled chicken breast;
- boiled veal (beef);
- boiled rabbit meat;
- turkey (also boiled);
- boiled sea fish fillet;
- light chicken broth;
- oatmeal and rice broth;
- yogurt without sugar and additives (from the second week of the diet);
- kefir 1% fat (from the second week, if there is no diarrhea);
- raw yolk of a chicken or quail egg (from the second week);
- raw beef (from the third week of the diet);
- raw chicken fillet (third week);
- low-fat cottage cheese (at the end of the diet)
As mentioned above, all products must be ground to a pate consistency. Raw meat is given at the end of the diet, if the pet is clearly on the mend. Milk should not be given. Food should never be of questionable freshness or quality.
Products that are prohibited
In order for the cat to be healthy and not suffer from gastritis, the following products should never get into his bowl::
- salt, sugar;
- pepper and any other spices;
- onions (it causes anemia);
- fatty meat (pork, lamb);
- bones;
- production waste – chicken feet, heads, skin;
- smoked meats;
- yeast dough and flour products in general;
- milk;
- starch.
It is useful to periodically replenish the reserves of vitamins and minerals in the cat’s body. They are especially needed for a speedy recovery and when dieting. Balanced vitamin complexes for cats will help compensate for the lack of nutrients. They should be purchased exclusively from a veterinary pharmacy.
Important: vitamins produced for humans should not be given to cats.
Prevention
To avoid having to treat gastritis in a cat, it is important to know how to prevent it:
- Correct feeding regimen. You should not give your pet anything from your table. The number of feedings should be individually selected. The food should not be too hot or too cold, and of course it should be fresh;
- Prevention of poisoning. It is necessary to hide from your pet all household chemicals, cosmetics, all kinds of perfume additives, oils, medicines, etc. The pet, of course, will not lick the floor after you have washed it with bleach, but it will walk across it and then definitely lick its paws , so wash such substances off the floor after cleaning. Indoor plants also need to be put out of reach of the pet;
- Remove all small items. Cats often swallow bags, threads, ropes, etc. while playing;
- Do not self-medicate. There are a number of drugs intended for people, but contraindicated in cats. And those drugs that are indicated for cats can be prescribed in a different dosage than for humans;
- Prevention of infections and invasions. Regular vaccination. Timely treatment against parasites. Thermal treatment of products of animal origin. Restriction of access to the street;
- Timely visit to the veterinarian. If you have the slightest suspicion of abnormalities in your pet’s well-being, you should contact a specialist in order to begin treatment in a timely manner.
Preventive measures
The main preventive measure is to ensure a balanced diet. Make sure your cat always has high-quality food. Missing foods, as well as the abuse of “human” foods, irritate the mucous membranes of the stomach.
You can prepare special food yourself (preferably based on poultry or lamb) or buy it in specialized pet stores. Make sure your cat does not have access to household chemicals.
Do not forget to regularly treat for worms. This applies even to those animals that are never outside! Be more attentive to the condition of your beloved pet and at the first signs of gastritis, immediately contact a professional veterinarian!