Animals, like humans, often suffer from allergic reactions. The pathological condition occurs as a result of various factors, but in the vast majority of clinical cases, an allergy occurs to food. As a result of the penetration of foreign protein components included in cat food into the pet’s body, a response occurs.
The body's defenses recognize the allergen and begin to attack it, thus trying to eliminate it. A specific reaction occurs, manifested by a general discomfort, itching and apathy. The development of the reaction directly depends on the state of the immune system. A weakened animal’s body can perceive even familiar food as dangerous, giving signals in the form of an allergy.
Signs of food allergies in cats
Food allergies in cats are usually manifested by a whole bunch of various symptoms, the most typical of which are itching, redness or rash on the skin.
Animals often experience profuse discharge from the eyes and ears, leading to the appearance of conjunctivitis and otitis. In advanced cases, allergies lead to baldness of entire areas of the skin, the appearance of ulcers, which are complicated by secondary infection and turn into eczema.
Food intolerance or allergy?
Sometimes food allergies cause vomiting and upset bowel movements, which is why it is confused with food intolerance. However, food intolerance is precisely a violation of the digestion of a certain type of food due to a lack of enzymes, metabolic disorders and other functional disorders.
Food intolerance manifests itself immediately, and most often only with digestive disorders. But food allergies are cumulative in nature, and its symptoms may appear several months or even years after consuming food containing the allergen.
Clinical cases
A case of food intolerance in the cat Steve
Brief anamnesis
- Scottish fold cat breed
- Age – two years
- I was admitted with an excoriation on my head.
- Lives at home
- No contacts
- People are healthy
- From the moment of acquisition until the visit to the clinic, the animal had no problems with its skin, and the owners’ skin was also fine. In general, Steve’s life has not changed in any way, except for one detail - two days ago the owners changed their diet.
Treatment
- Bearing in mind that itching in the head area can develop against the background of food, non-food hypersensitivity, against the background of flea allergies, we have prescribed an algorithm for itching
- LUM: “—”
- Scrapings: "—"
- Trichogramma: "—"
Recommendations
- Metypred (05 mg/kg × after 12 hours)
- Treatments against parasites
- Elimination diets
Steve recovered
After 2 weeks, the owners came for an appointment. And they reported that the itching went away on its own. At the same time, they did not do anything, they decided to just watch their pet. And switching to the previous diet was enough to solve the problem. We believe that in this case, we were talking about food intolerance, which developed quickly, apparently without the formation of immune mechanisms, and as a result of direct exposure to some food ingredients. When the animal was switched to its previous diet, the problem was stopped.
Allergy to airborne allergens in Bruni
Brief anamnesis
- Breed: Don Sphynx
- Age 2 years
- Lives at home
- There is a cat at home, she has no skin problems
- No contact with other animals
- People don't get sick
- Complaints: itching of the head and neck area; scratches on the head and body
- Prior to presentation, antibiotic therapy was administered, apparently due to secondary bacterial lesions at the sites of excoriation
- Despite the history, we did consider infections such as notoedrosis, demodicosis (caused by gata), and dermatophytosis. However, these diff. the diagnoses seemed unlikely because there was another cat in direct contact and she had no health problems. To a large extent, we assumed that there were variants of hypersensitivity.
Diagnostics
- Scrapings - negative
- Sowing for fungi - the growth of dermatophytes is not determined
- Biopsy - large number of eosinophils
- Elimination diet – itching persists
- Flea treatment – itching persists
- Blood test in ELISA. The animal was found to have antibodies against fleas and the Akarus Siro household dust mite.
Diagnoses
- Allergy to flea saliva
- Allergy to household allergen Acarus Siro
Therapy
- Cyclosporine 5 mg/kg, daily
- Vaccination with a significant allergen
- By the end of the first year of vaccination, we managed to eliminate cyclosporine almost completely. Brunya receives 2 capsules per week, with an interval of 1 time in 3 days. And solely to reassure the owner. Probably, soon we will be able to completely abandon cyclosporine.
- Flea treatments - every 14 days
The body's immune response
The thing is that food allergy is a disease associated with the immune system; it is caused by an inadequate reaction of the immune system to certain proteins of animal or plant origin.
As a result, an immune response occurs in the form of the production of histamines, which are designed to fight substances perceived by the body as foreign. Also, the cumulative nature of allergies is the reason that the allergens are those proteins that the cat most often receives from food.
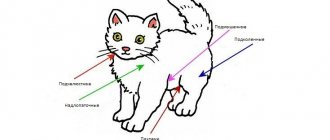
Diagnostics
The effectiveness of treatment depends on the accuracy of the examination of the pet. The appearance of skin lesions, bald patches, and frequent itching is a serious reason to visit a veterinarian. Particular attention is paid to the presence of parasites - fleas, lice eaters, ticks; their presence requires additional treatment. To determine the allergen, a method of excluding probable antigens is used.
If an allergic reaction occurs once a year during a certain season, the allergen is not looked for. Seasonal allergies are treated with antihistamines, which should be given until the antigen is completely eliminated.
It should be borne in mind that such a diagnosis and appropriate treatment can only be prescribed by a specialist. After a detailed diagnosis and collection of anamnesis from the owner’s words. Allergies in their symptoms are in many ways similar to infections and inflammation of internal organs.
Common allergens for cats
Some of the foods that most commonly cause allergic reactions in dogs and cats include:
- chicken's meat;
- beef;
- mutton;
- fish;
- dairy products;
- soy;
- corn;
- wheat.
Allergies can be caused by one product or several at once. Sometimes changing food does not bring results, since only the meat component of the food changes, but the base remains unchanged - corn and wheat, which are contained in a large number of feeds.
Features of allergies to non-stinging insects
What is the prevalence of insect allergies? What insects cause allergies? What are the methods of emergency treatment and prevention?
The concept of “insect allergy” (IA) implies the occurrence of allergic reactions upon contact with insects and their metabolites: upon contact with them, inhalation of particles of the body of insects or their metabolic products, bites, stings by insects. This type of allergy is called insect according to the name of the class - Insecta.
AI can play the role of a trigger factor in the formation of bronchial asthma, allergic dermatoses, Quincke's edema, and can also cause anaphylactic shock.
The most common causes of allergies are bites of blood-sucking insects (mosquitoes, etc.), stings by bees, wasps and other representatives of the order Hymenoptera, as well as contacts with “indoor” insects in house dust (cockroaches, micromites, flies, moths, window ants and etc.) and their metabolites. The severity, severity, and suddenness of the manifestation of allergic reactions (up to the occurrence of anaphylactic shock with a fatal outcome) to insect allergens require the development of methods for reliable prevention and effective treatment of these conditions.
Representatives of the insect fauna spread over considerable distances not only through active flight, but also through passive transfer by wind, as well as by fixation on the skin of an animal or person. The accumulation of insects depends on environmental factors: temperature, humidity, atmospheric pressure, wind force, etc. In entomologically unfavorable areas, the likelihood of stings, bites and contacts with insects and their metabolites is very high [1].
All types of insects, according to the method of introducing their allergens into the human body, can be conditionally divided into two large groups: stinging (representatives of the order Hymenoptera-bees, wasp, ants-bees, wasps, ants, etc.) and non-stinging (representatives of 12 orders of the Insecta class: Lepidoptera - butterflies; Dyctioptera - cockroaches; Diptera - mosquitoes, flies; Orthoptera - grasshoppers, crickets; Ephemeroptera - May fly, etc.; Coleoptera - beetles; Siphonaptera - fleas; Trichoptera-Caddis flies, Psocoptera - book louse, etc.) [3 ].
Non-stinging insects (NS) can also be divided into groups: non-biting (Chironomidae - bloodworms, etc.), biting (Cockroach - cockroaches, etc.), blood-sucking (Mosquitoes - mosquitoes, mosquitoes, etc.).
Prevalence of allergy to NN
Despite numerous publications concerning the allergenic effects of insects and their metabolites, the main attention of most researchers has been focused on the effects of the venom of stinging insects [2, 8, 9, 10, 12, 13]. However, given the widespread prevalence of NN in the environment, the impossibility of predicting contacts of patients with allergic diseases with these types of insects and the severity of allergic reactions to NN allergens, the study of the clinical issues, pathogenesis and treatment of allergic conditions caused by the action of NN allergens is of particular importance. This study is devoted to the analysis of the impact of NN allergens on the human body.
As an example of a source of human sensitization among the so-called non-biting NNs, one can name bloodworms belonging to the class Chironomidae. The International Allergen Nomenclature (IUIS) lists 16 allergens of this insect. Chironomidia are found in various parts of the world, but are most common in regions where there are open bodies of water [1, 3]. They are often united by one name - bloodworms, which in dried form are used as food for aquarium fish. There are three ways that a person can come into contact with this allergen: airborne insect particles can land on the mucous membranes of the respiratory tract when cutting fresh fish, when feeding aquarium fish, or when a person bathes in rivers and lakes. The last example explains cases of skin manifestations of allergies in the form of rashes, itching, etc. in some individuals after swimming in open water. With a wide variety of these insects, Chironomus thummi-thummi should be noted among the most “allergenic” species. In general, according to the observations of a number of authors [3, 14], allergy to NN is especially common in England, Germany, Italy, Japan, Sweden, and the USA [5, 6, 15].
Among the insects that live near lakes, large rivers and other open bodies of water in a number of regions of the world, May flies (genus Ephemeroptera) are often found. More than 2000 species of these insects are known, of which inhalation allergies are caused by Ephemera vulgata, E.guttulata, Heptagenia longicauda, Ephemerella notata, etc. In 1913, the first report of sensitization to May flies was published [16]. It was further confirmed [11] that the cause of bronchial asthma can be an allergy to May flies. According to the data obtained, in 7% of 1248 patients with atopic diseases examined by the scientist, the source of sensitization was the allergens of these insects.
A separate group of insects belonging to the order Orthoptera includes the well-known grasshoppers, crickets, and locusts. A number of studies have shown that these insects have an allergenic effect on the human body. Immediate reactions to Crickets cricket allergens have been reported [3, 17]. Clinical manifestations were noted in the form of bronchospasm and rhinoconjunctival syndrome upon contact with insects. Hypersensitivity to cricket allergens was confirmed by the presence of positive skin tests, as well as by determining specific IgE antibodies to these insect allergens.
Allergic reactions to contact with grasshoppers were detected in two research laboratory employees [18] who had contact with Melanoplus sanguinipes. The possibility of allergy to locusts has been proven in a number of studies [19].
Each insect species has its own ecological niche, its own habitat, which must correspond to the life support processes of the insect individuals that make up this species. The quality of the environment supports the viability of the insect and provides all the conditions for its reproduction. Communities of insects appear that inhabit certain areas. In particular, the insect fauna of a human home has a certain species composition. The so-called indoor insects include the cockroach, bedbug, book louse, moth, etc. Numerous studies by entomologists and allergists conducted over the years [20, 21] have shown that of the entire species diversity, for example cockroaches (and there are more than 3500 species of these insects), only a few have allergenic activity towards the human body. For Russia, the most relevant (Fedoskova T.G. et al., 1996) are Blattella germanica, Periplaneta Americana and Blatta orientalis. In 33% of patients suffering from atopic bronchial asthma and having hypersensitivity to house dust, sensitization to cockroach allergens was confirmed by the occurrence of asthma attacks when cleaning in places where insects accumulate, as well as the presence of positive results when conducting skin testing with cockroach allergens, and the presence of specific IgE antibodies to these insect allergens in blood serum samples of the examined patients.
Allergens of cockroaches and locusts are cross-reactive [7], which may cause the occurrence of cross-allergic reactions to the allergens of these insects.
Finally, there are so-called blood-sucking insects, the development cycle of which (mainly in females) requires the presence of blood. Insects are grouped into this group according to the indicated method of contact with humans. This includes representatives of different species, even different families. These are representatives of the families Culicidae (mosquitoes), Liposcelidae (lice), Pulicidae (fleas), etc. [4].
Mosquitoes are typical representatives of blood-sucking insects. As shown by the work of A.D. Ado et al. (1995), V. N. Fedoseeva et al. (1998-2000), the greatest danger to the taiga and steppe regions of Russia is represented by Aedes aegypti and Culex pipiens. The presence of allergens in the saliva of mosquitoes, which stimulate an active allergic response, has been established. It was possible to dissect the salivary glands of insects and isolate antigenic fractions; When they were then introduced under the skin of sensitized individuals, local allergic reactions were observed. 12 polypeptides were isolated from the saliva of the mosquito Aedes aegypti (Mosguitoes) and their allergenic properties were proven [3].
Thus, it is quite obvious that NHs, on the one hand, are the most common representatives of the insect fauna of the Earth, and on the other hand, the allergenic activity of most of them, as well as their etiopathogenetic significance in the formation of various forms of allergic diseases, has been proven.
Clinical manifestations of allergy to NN
Individuals who are not sensitized to insect allergens usually experience only symptoms of a local reaction to a bite: redness, burning, itching. Sensitized individuals may develop both a pronounced local reaction and a systemic one (up to anaphylactic shock with possible death). Clinical manifestations of allergies are characterized by severity, severity, and suddenness of reactions. The occurrence of an allergic reaction can occur in both adults (most often between the ages of 16 and 35) and children. Allergic reactions to the bites of blood-sucking insects are detected in 17-20% of people suffering from atopic diseases [2].
In patients who are hypersensitive to mosquito bites, a full-blown allergic local reaction is usually detected in the form of swelling, severe redness, and the formation of papular or blistering elements on the skin at the site of the bites. Inappropriate reactions to the bite of one insect occur: from gigantic infiltration at the site of the bite, which persists for 3-4 weeks, to systemic manifestations in the form of a generalized rash, attacks of suffocation. Often, scratching of bite sites becomes infected with bacterial flora. Bites of blood-sucking insects (fleas, mosquitoes, etc.) rarely cause anaphylactic shock, but such cases have been reported in the literature.
In case of multiple bites, signs of intoxication may be observed: rise in body temperature, fever, headache.
Noteworthy is the different sensitivity of different population groups to the bites of blood-sucking insects. The population of taiga regions, which has long-term contact with mosquitoes and midges, is, as a rule, more resistant to their bites due to the immune defense that is formed through repeated insect bites.
Allergic reactions to the bites of blood-sucking insects from representatives of the order of bedbugs (order Hemiptera) that live in human homes are an important problem for some regions. For example, a bite from the “kissing bug” Triatoma protracta can provoke not only a local allergic reaction, but also severe systemic anaphylactic reactions. Clinical manifestations of an allergy to the bites of these blood-sucking insects are characterized by the formation of papules with a dark dot in the center at the site of skin lesions, then vesicles 2-3 cm in size [1].
Bed bugs also cause allergic reactions. The sensitivity of patients to a bite depends on the number of bites and the type of bedbug (sensitization to bedbug bites develops slowly). The clinical picture of an allergic reaction develops rapidly after a bite from one individual. The interval between the bite and the development of symptoms in most cases ranges from 0-10 minutes to 40 minutes. After a few hours, the severity of local symptoms may increase: dense swelling that covers a wide area (from joint to joint), itching, hyperemia, and sometimes local hyperthermia. It is also possible that local manifestations of the late phase of an immediate type allergy may occur - 4-6 hours after the bite. There is a different dynamics of the manifestation of an allergic reaction to a bite: it occurs after 6-12 hours, increases within 48 hours, the nature of the course is recurrent, sometimes up to 2 months, manifestations of papular and sometimes vesicular or bullous rash may occur. Systemic reactions are also noted in the form of a generalized urticarial rash (sometimes of a confluent nature), Quincke's edema, and bronchospasm. In some cases, loss of consciousness, swelling of the eyelids, tongue, larynx, bronchospasm are observed, and anaphylactic shock develops. This type of allergy often develops as an immediate type.
Similar skin manifestations can be observed after bites of mosquitoes, midges, and midges. These reactions are represented by three types of skin rash: an acute erythematous reaction, reminiscent of erysipelas, but without fever and enlargement of peripheral lymph nodes; vesicular bullous; necrotic rash resulting in scarring. With severe local reactions, general intoxication phenomena may also occur in the form of headache, nausea, chills, sweating, dry mouth, and insomnia.
Representatives of the order of butterflies (Lepidoptera) can cause manifestations of dermatitis such as urticaria. The reaction usually occurs in a slow manner. Application tests with extracts of the bodies of caterpillars, butterflies, and gypsy moth filaments are registered after 24-48 hours, and skin tests with allergens from the bodies of caterpillars in 88% of cases give a positive result after 0.5-12 hours.
In world clinical practice, there are known cases of outbreaks of allergic diseases of the bronchopulmonary system in people living near water during the accumulation of insects from the order of caddisflies in water bodies.
Beetles (order Coleoptera) - agricultural pests induce allergic reactions in dockers unloading ships with contaminated products, warehouse and granary workers. Hypersensitivity to beetle allergens can clinically manifest itself in the form of symptoms of allergic rhinitis, conjunctivitis, and provoke attacks of suffocation. The literature contains data on cases of skin manifestations such as urticaria upon contact with beetles and larvae of Dermes maculatus Degeer.
Cases of allergies to migratory locusts (order Orthoptera) have been recorded in places where these insects accumulate. Insect feces have the greatest allergenic activity. Clinically, this condition manifests itself in the form of allergic rhinitis and asthma attacks. The locust allergen is classified as aggressive, since it gives a positive skin reaction in patients during a specific examination with the allergen at a high degree of dilution [9, 10]. IgE and IgG antibodies specific to locust allergens were detected in the blood serum of patients.
Diagnosis of allergy to NN
Diagnosis of local allergic reactions is usually difficult due to possible manifestations of a toxic type of reaction, especially in individuals with autoimmune and oncological diseases [2]. The possibility of a local reaction as a manifestation of an infectious process (the pathogen is transferred with the saliva of the insect) cannot be ruled out. Sometimes the elements of the rash with local manifestations of this type of allergy are similar in nature to the elements of the rash with prurigo (prurigo).
The clinical picture of the disease and the results of specific examination methods are decisive.
Evidence of insect allergy:
- connection between clinical manifestations of allergies and insect bites;
- the presence of positive skin tests with extracts from the bodies of insects and their metabolic products;
- the presence in the blood serum of patients of specific IgE antibodies to these insect allergens.
When collecting an allergy history, it is necessary to find out whether the patient has previously been exposed to insect bites, determine the severity of reactions, the duration of clinical manifestations, and, if possible, the type of insect, and evaluate the effectiveness of using anti-allergic medications. In addition, it is necessary to find out whether there are any cases of allergic reactions in the anamnesis upon contact with other insects, including reactions to stings from representatives of the order Hymenoptera (wasps, bees, etc.). History data regarding the intensity of the local and systemic reaction to the insect bite should also be carefully assessed.
The strategy for further diagnosis is determined based on medical history. If there are pronounced clinical manifestations of an anaphylactic reaction to an insect bite, in vitro laboratory diagnostic methods with a causally significant insect allergen should be used. The purpose of diagnosis is to identify specific IgE antibodies in the patient’s blood serum. Determination is carried out by enzyme immunoassay or chemiluminescent analysis.
Skin tests are recommended to be performed with caution and no earlier than 2-3 weeks after the development of a systemic reaction. The method of allergometric testing (prick test or intradermal test) is selected taking into account the patient’s individual sensitivity to the insect allergen (according to the allergy history). The skin reaction should be assessed after 20 minutes, 6, 24 and 48 hours.
Treatment
Treatment involves symptomatic treatment of acute reactions and preventive pre-season specific hyposensitization with extracts of insect allergens. Treatment of local reactions to bites of blood-sucking insects with hypersensitivity to allergens of stinging hymenoptera is carried out identically. Considering, however, the increasingly prevalent reactions of transient and delayed types of tissue damage in this form of allergy, patients are prescribed calcium and rutin preparations to reduce vascular permeability, and, if necessary, undergo more active glucocorticosteroid therapy. Treatment of general allergic reactions to blood-sucking insect bites is carried out taking into account the type of reaction. To relieve a general reaction of an immediate type, adrenaline, dexamethasone or prednisolone, antihistamines are used first; in case of bronchospasm, a 2.4% solution of aminophylline is used intravenously; other drugs are prescribed according to indications. The doses of administered drugs depend on the severity of clinical manifestations. Adrenaline is not used to relieve transitional (slow) type reactions. They mainly use corticosteroids, antihistamines, and calcium supplements. Doses and treatment regimens are selected according to the severity of the reaction and the number of relapses [2].
If a patient is diagnosed with an allergy to blood-sucking insects, some measures are recommended to eliminate the risk of developing an anaphylactic reaction if a repeated insect bites: in the summer months, before going to the forest, to places located near water areas, it is necessary to treat clothing and, if possible, skin with repellents or carry fast-acting aerosol insecticides with you. You should also always keep with you emergency aid for insect bites (syringe, adrenaline, prednisolone or dexamethasone, suprastin).
In the autumn-winter period, the patient is prescribed a course of specific immunotherapy (SIT) with water-salt extracts of allergens. SIT is a method of pathogenetic therapy that reduces the body's hypersensitivity to saliva, insect body parts and their metabolites. Immunotherapy is carried out with an allergen from the bodies of mosquitoes, the activity of which is tested by protein (PNU). In some cases, when elimination of indoor allergens, including cockroach allergens, is impossible, SIT is carried out. The effect of specific treatment in clinical practice in patients with general reactions to mosquito bites was noted in 70% of cases [2].
Thus, the wide prevalence of AI in different regions, the severity of clinical manifestations of allergic and other reactions to the bites of these insects, the absence in practical allergology of a wide range of diagnostic and therapeutic forms of insect allergens - all this gives reason to talk about the relevance of the problem posed, which is both medical, and social nature, as well as the need to strengthen preventive measures, timely diagnosis and treatment of these conditions.
For questions about literature, please contact the editor
Cat food for food allergies
There is no test for food allergies in cats, and the only accurate way to determine which component is causing it is an elimination diet. It consists of sequentially eliminating one food after another and monitoring symptoms for six weeks.
If the signs of allergy begin to weaken, then we can conclude that it is the excluded component that is the cause of the disease. But only the result of a provocative diet will give complete confidence, when after some time the suspected ingredient is introduced into the diet again, and as soon as signs of an allergy appear, it becomes finally clear who the culprit is.
As you can see, this process is lengthy and difficult to implement, given that there are a lot of components in ready-made feeds and in practice it will not be possible to eliminate each of them. But knowing which ingredients cause allergies most often, you can try to act differently.
First of all, exclude grains by choosing grain-free food, after carefully studying its composition. The diet should not only contain flour, but also isolated sources of vegetable protein, which may be hidden under the name “gluten”.
Acana food for cats with allergies
In the Acana line of cat food you will find only such diets - without the slightest content of vegetable protein in any form. If excluding only grain products does not give the desired effect, then the reason is in the source of animal protein.
We advise you to try introducing ACANA Pacifica, which contains only fish, into your cat's diet. There are very few all-fish dry diets on the market, so most likely this will be a completely new type of protein for your cat.
And to exclude allergies to red meat - lamb or beef, ACANA Wild Prairie food with turkey and chicken is suitable.
After choosing the most suitable food for cats with food allergies, exclude all additions from the cat’s diet - cat treats, tasty morsels from the table, natural products. It is very important that your cat eats only one type of food you choose for 6 weeks. If during this time the manifestations of allergies have disappeared, the type of food has been chosen correctly.
Which cats are more likely to suffer from chicken allergies?
There are some factors that can contribute to a cat becoming allergic to chicken:
- constant use of the product;
- genetic predisposition;
- problems with the digestive tract;
- other types of allergies.
Meat proteins are fermented in the stomach and intestines, breaking down into short peptides and amino acids. If digestion for any reason becomes inadequate, then the intestinal walls capture larger protein particles, to which the animal’s immune system reacts.
Chronic intestinal inflammation often contributes to the development of food intolerances. There is also a reverse relationship: with a constant supply of a product that causes an allergy, an inflammatory process develops in the intestinal wall.
As for other types of allergies, they contribute to increased allergic reactions to chicken. Thus, the presence of hypersensitivity to flea bites (and even apartment cats are not immune from this nuisance) and atopic dermatitis (reaction to external irritants) can enhance the body’s reaction to food irritants.
Treatment
The main thing in the treatment of allergies is eliminating the allergen. Preventive measures are reduced to eliminating the antigen and symptoms of the immune response; they are chosen depending on the allergen group:
- household and book dust – systematic wet cleaning of the premises
- mold – control room humidity, limit pet’s access to damp areas (basement, cellar), avoid walking after rain
- pollen – limit the animal’s access to the street during the period of distribution of pollen grains, washing the cat
- blood-sucking microorganisms (fleas, lice eaters, etc.) – additional treatment of the pet’s skin, sanitation of the room
- household chemicals - use of hypoallergenic shampoos
- food allergy – selection of suitable food excluding the product that causes the reaction
In the absence of the desired effect of preventive measures, antihistamines are prescribed. Suprastin, clemastine, bravegil, etc. are used. The treatment period, dose and amount of medication taken are determined individually, depending on the weight and characteristics of each pet. Skin lesions require additional treatment to avoid secondary infection.